Recrudescent typhus, also known as Brill-Zinsser disease, is a late relapse of epidemic typhus caused by Rickettsia prowazekii. This condition typically arises years after the initial infection, often when the immune system is compromised. Although less severe than primary epidemic typhus, recrudescent typhus poses serious health risks if not properly identified and treated.
Causes and Risk Factors of Recrudescent Typhus
The causative agent, Rickettsia prowazekii, remains dormant within the human body after the primary infection. It can reactivate later, particularly during periods of immunosuppression, aging, or chronic illnesses. Individuals with a history of epidemic typhus are at risk. Factors such as poor living conditions, malnutrition, and lack of access to healthcare increase susceptibility.
Clinical Manifestations and Symptoms
Recrudescent typhus presents with a range of nonspecific but notable symptoms, including:
- Sudden onset of fever
- Severe headache
- Chills and rigors
- Myalgia (muscle pain)
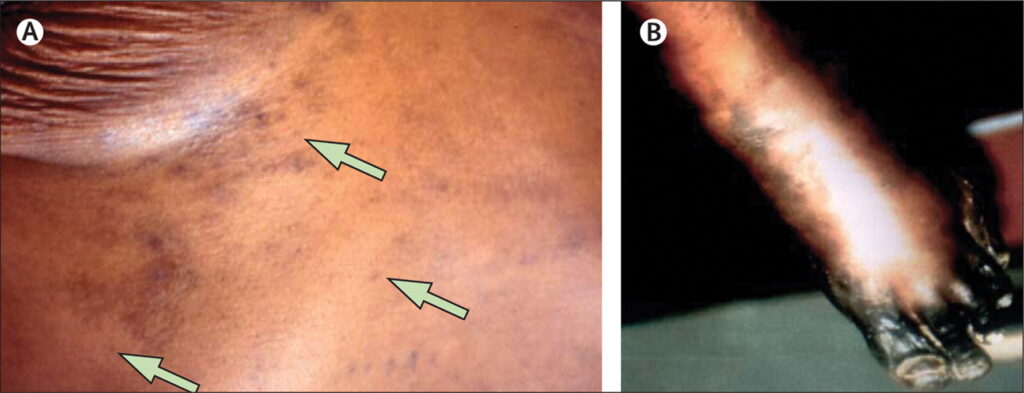
- Rash, typically appearing later
- Generalized weakness
- Cough and photophobia in some cases
Unlike primary epidemic typhus, the rash is often less pronounced, and the disease course is usually milder, though complications can still arise.
Pathophysiology of Recrudescent Typhus
Upon reactivation, dormant R. prowazekii organisms begin multiplying within endothelial cells, causing widespread vasculitis. This inflammatory process disrupts vascular integrity, leading to the characteristic symptoms such as rash, fever, and systemic inflammation. If untreated, complications like myocarditis, encephalitis, or renal failure may develop.
Diagnostic Approach for Recrudescent Typhus
Accurate diagnosis relies on clinical suspicion, especially in patients with a history of epidemic typhus. Key diagnostic steps include:
- Clinical Evaluation: Assessment of symptoms and medical history.
- Serology: Detection of antibodies using indirect immunofluorescence assay (IFA).
- Polymerase Chain Reaction (PCR): Identification of R. prowazekii DNA in blood samples.
- Histopathology: Biopsy of rash lesions if necessary.
Timely diagnosis is essential to initiate effective treatment and prevent complications.
Effective Treatment Modalities
The cornerstone of recrudescent typhus treatment is antibiotic therapy:
- Doxycycline: The first-line antibiotic, typically 100 mg orally twice daily for 7–14 days.
- Chloramphenicol: An alternative for patients with contraindications to doxycycline.
Supportive care measures, such as hydration, fever control, and monitoring for complications, are also critical. Prompt initiation of therapy leads to rapid symptom resolution and excellent prognosis.
Preventive Measures and Public Health Considerations
Preventing recrudescent typhus primarily involves:
- Improving living conditions and hygiene
- Controlling lice infestations, as lice can serve as vectors in initial infections
- Early treatment of primary typhus cases to prevent future recrudescence
- Vigilant monitoring of at-risk populations, especially in endemic regions
Public health initiatives focusing on vector control and community education are vital in minimizing the disease burden.
Recrudescent typhus remains a significant clinical concern, particularly in populations with prior exposure to epidemic typhus. Early recognition, accurate diagnosis, and prompt antibiotic treatment are essential to ensuring favorable outcomes. Continued public health efforts in prevention and education are crucial in reducing the incidence and impact of this relapsing infection.

