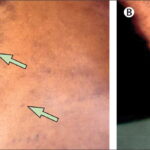
Raynaud’s phenomenon is a vascular disorder characterized by episodic constriction of small arteries, leading to reduced blood flow to extremities, primarily fingers and toes. Triggered commonly by cold exposure or emotional stress, this condition manifests through distinct color changes in the skin — typically white, blue, and then red as blood flow returns.
While not inherently life-threatening, Raynaud’s phenomenon can severely impact quality of life and, in secondary cases, signal underlying systemic diseases.

Types of Raynaud’s Phenomenon
Raynaud’s phenomenon is broadly categorized into two types, distinguished by underlying causes and severity.
Primary Raynaud’s Phenomenon
Primary Raynaud’s, also known as Raynaud’s disease, occurs independently without any associated medical condition. It is more common and generally less severe. Individuals with primary Raynaud’s often experience mild symptoms that can be managed through lifestyle modifications.
Secondary Raynaud’s Phenomenon
Secondary Raynaud’s, also referred to as Raynaud’s syndrome, is linked to underlying health disorders such as scleroderma, lupus, or rheumatoid arthritis. This form tends to be more serious, potentially leading to skin ulcers or tissue damage if left untreated.
Causes and Risk Factors of Raynaud’s Phenomenon
Understanding the causative factors behind Raynaud’s phenomenon is essential for effective management and prevention.
1. Primary Raynaud’s Causes
- Genetic Predisposition: A family history of Raynaud’s increases susceptibility.
- Environmental Factors: Cold climates and sudden temperature drops are significant triggers.
- Demographic Factors: It predominantly affects women aged 15 to 30.
2. Secondary Raynaud’s Causes
- Connective Tissue Diseases: Conditions such as scleroderma, lupus, and rheumatoid arthritis are strongly associated.
- Arterial Diseases: Atherosclerosis and Buerger’s disease can contribute.
- Repetitive Actions: Occupational factors like typing or using vibrating tools can increase risk.
- Medications: Beta-blockers, chemotherapy agents, and migraine medications may induce or exacerbate symptoms.
Symptoms of Raynaud’s Phenomenon
Symptoms typically manifest episodically and vary in intensity and frequency among individuals.
- Color Changes: The hallmark symptom involves color transitions—pallor (white), cyanosis (blue), and hyperemia (red).
- Numbness and Tingling: Affected areas may feel numb or prickly during and after an episode.
- Pain or Throbbing: Discomfort often follows when blood flow returns to the extremities.
- Cold Sensitivity: Even mild drops in temperature can trigger symptoms.
In severe secondary Raynaud’s, patients may develop skin sores, ulcers, or, rarely, gangrene.
Diagnosing Raynaud’s Phenomenon
A thorough evaluation is crucial to distinguish between primary and secondary forms.
1. Medical History and Physical Examination
A detailed history focusing on symptom patterns, family history, and associated diseases helps guide the diagnosis.
2. Nailfold Capillaroscopy
This non-invasive test examines tiny blood vessels near the fingernails under a microscope. Abnormalities can suggest secondary Raynaud’s linked to connective tissue diseases.
3. Blood Tests
- Antinuclear Antibodies (ANA): Positive results may indicate autoimmune diseases.
- Erythrocyte Sedimentation Rate (ESR): Elevated ESR can signal systemic inflammation.
- Specific Autoantibodies: Tests for scleroderma-related antibodies may be performed if secondary Raynaud’s is suspected.
Treatment Strategies for Raynaud’s Phenomenon
Management of Raynaud’s phenomenon focuses on reducing frequency and severity of attacks, preventing tissue damage, and treating underlying diseases when applicable.
1. Lifestyle Modifications
- Cold Protection: Wearing gloves, thermal socks, and layered clothing.
- Stress Management: Techniques such as meditation and biofeedback can reduce frequency.
- Smoking Cessation: Smoking restricts blood vessels and worsens symptoms.
2. Pharmacological Treatments
- Calcium Channel Blockers: Medications like nifedipine help dilate blood vessels and reduce attack frequency.
- Vasodilators: Drugs such as nitroglycerin cream applied to affected areas promote blood flow.
- Phosphodiesterase Inhibitors: Sildenafil has shown benefits in severe cases.
3. Surgical Options
In rare, severe cases:
- Sympathectomy: Surgical interruption of nerves controlling blood vessel constriction may be considered.
- Digital Ulcer Debridement: Surgical care of ulcers to promote healing and prevent infection.
Preventing Raynaud’s Phenomenon Flare-Ups
Proactive strategies can minimize episodes and enhance quality of life.
- Thermal Precautions: Dress warmly in cold environments and pre-warm vehicles and homes.
- Emotional Regulation: Stress reduction techniques can help prevent emotional triggers.
- Avoid Caffeine: Caffeine can constrict blood vessels and exacerbate symptoms.
- Regular Exercise: Promotes overall vascular health and circulation.
Living with Raynaud’s Phenomenon
Individuals with Raynaud’s can lead healthy, active lives with appropriate management. Early diagnosis, patient education, and adherence to preventive measures are vital for minimizing complications. It is essential for those affected to remain vigilant about skin care, promptly address any sores or ulcers, and maintain regular follow-up with healthcare providers.
Raynaud’s phenomenon is a manageable vascular disorder characterized by episodes of reduced blood flow to extremities. Differentiating between primary and secondary types is essential for appropriate treatment and monitoring. Through a combination of lifestyle adjustments, medication, and, when necessary, surgical intervention, individuals can effectively control symptoms and prevent complications. By fostering awareness and adopting preventive strategies, we can significantly enhance the well-being of those living with Raynaud’s phenomenon.