Radiation-induced mucositis is a common and debilitating complication resulting from radiation therapy, especially in the treatment of cancers in areas such as the head, neck, and chest. It manifests as painful inflammation and ulceration of the mucosal lining in the mouth, throat, and other parts of the digestive tract. As a consequence of radiation treatment, mucositis can significantly impact a patient’s quality of life, leading to difficulties with eating, speaking, and swallowing. In this article, we will provide a detailed exploration of radiation-induced mucositis, its underlying causes, clinical features, preventive measures, and treatment options.
Understanding the Causes of Radiation-Induced Mucositis
Radiation therapy works by targeting and destroying cancer cells. However, the radiation can also affect healthy tissues, particularly rapidly dividing cells like those found in the mucosal lining of the oral cavity. The development of mucositis occurs as a result of direct DNA damage to these cells, leading to inflammation, cell death, and disruption of the mucosal barrier. Several factors influence the severity of radiation-induced mucositis:
- Radiation dose and volume: Higher doses and larger areas of radiation are directly correlated with more severe mucositis.
- Location of treatment: Radiation to the head, neck, and throat areas increases the risk of mucosal damage in the oral cavity and upper digestive tract.
- Chemotherapy concurrent with radiation: Chemotherapy agents can further exacerbate mucositis by suppressing immune function and enhancing radiation-induced damage.
- Individual patient factors: Age, general health, and prior oral health status (e.g., existing dental issues) can all impact the severity and duration of mucositis.
Symptoms and Clinical Features of Radiation-Induced Mucositis
The symptoms of radiation-induced mucositis can vary from mild irritation to severe ulceration. The clinical features typically appear 1–2 weeks after radiation therapy begins, with the severity peaking around the third week of treatment. Common signs and symptoms include:
- Pain and burning sensation in the mouth and throat
- Redness and swelling of the mucosal lining
- Ulceration and sores that may bleed when irritated
- Difficulty swallowing (dysphagia) and speaking (dysphonia)
- Dry mouth (xerostomia), often accompanied by thickened saliva
- Foul taste or halitosis
- Infection risk due to the loss of mucosal integrity
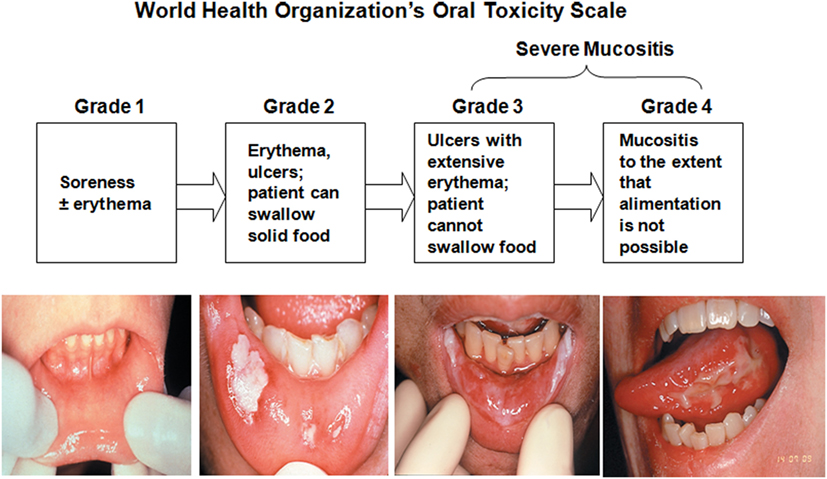
Staging of Mucositis
Radiation-induced mucositis is typically graded using the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE). The stages include:
- Grade 1 (Mild): Erythema or redness of the mucosa with no ulceration.
- Grade 2 (Moderate): Painful erythema and edema, with some ulceration but without the need for tube feeding.
- Grade 3 (Severe): Extensive ulceration requiring feeding tubes and significant pain.
- Grade 4 (Life-threatening): Severe ulceration and necrosis, potentially requiring hospitalization or more invasive interventions.
Prevention of Radiation-Induced Mucositis
While it may not always be possible to prevent mucositis entirely, there are several strategies that can minimize its severity and impact on patients undergoing radiation therapy.
1. Pre-Radiation Oral Care and Health Assessment
Ensuring optimal oral health before initiating radiation therapy is critical in reducing the risk of mucositis. Dentists and oncologists should evaluate and address existing dental problems, such as infections or untreated cavities, that may increase the likelihood of oral complications.
2. Hydration and Moisturization
Keeping the oral cavity moist is essential in reducing dryness and irritation. Patients are encouraged to drink plenty of fluids and use oral moisturizers (e.g., saline solutions, glycerin) to maintain moisture balance in the mouth.
3. Dietary Modifications
Patients may benefit from a soft, bland diet that avoids acidic, spicy, or abrasive foods that could further irritate the mucosa. A diet high in protein and vitamins can promote healing and immune function.
4. Use of Cryotherapy
For patients receiving radiation to the head and neck, cryotherapy (sucking on ice chips during radiation) has shown promise in reducing mucosal inflammation and cell damage by constricting blood vessels and limiting radiation exposure to the oral mucosa.
5. Pharmacologic Interventions
Medications like amifostine, a cytoprotective agent, may help reduce the severity of mucositis by protecting healthy tissue from radiation-induced damage.
Treatment Options for Radiation-Induced Mucositis
Effective management of radiation-induced mucositis focuses on alleviating symptoms and promoting healing of the affected mucosa. The treatment approach is multi-faceted and may include:
1. Pain Management
Pain relief is central to improving the patient’s quality of life during treatment. Common approaches include:
- Topical anesthetics: Products containing lidocaine or benzocaine can provide localized numbing and reduce pain during eating and speaking.
- Systemic pain medications: Non-steroidal anti-inflammatory drugs (NSAIDs) or opioids may be used for more severe pain.
2. Oral Care and Hygiene
Maintaining proper oral hygiene is critical to prevent secondary infections and enhance recovery:
- Gentle brushing with a soft toothbrush
- Rinsing with saltwater or antiseptic mouthwashes to reduce bacterial load
- Avoiding alcohol-based mouthwashes, as they may cause further irritation
3. Topical Treatments
Several topical treatments are available to help soothe and protect the mucosal lining, including:
- Hydrocolloid dressings: These provide a protective barrier to ulcerated areas.
- Aloe vera gel: Known for its soothing and healing properties.
4. Nutritional Support
Patients with severe mucositis may require enteral nutrition or feeding tubes to maintain adequate nutritional intake, particularly if swallowing becomes difficult.
5. Use of Growth Factors
Granulocyte-macrophage colony-stimulating factor (GM-CSF) and other growth factors may be used in clinical settings to promote mucosal healing and reduce inflammation.
Monitoring and Follow-Up Care
Regular monitoring is crucial to assess the progression of mucositis and adjust treatment plans as needed. Healthcare providers should evaluate the severity of symptoms and offer ongoing support through nutrition counseling, pain management, and psychological support.
Radiation-induced mucositis presents a significant challenge for patients undergoing cancer treatment, particularly those receiving radiation to the head, neck, and chest areas. Early intervention, preventive strategies, and effective management of symptoms can significantly improve patient outcomes. By understanding the causes, symptoms, and treatment options for mucositis, healthcare providers can better support patients throughout their cancer treatment journey, minimizing the impact of this debilitating side effect.

