Q fever endocarditis represents a severe and life-threatening manifestation of chronic Coxiella burnetii infection. It predominantly affects individuals with pre-existing heart valve abnormalities, prosthetic valves, or vascular grafts. Due to its subtle clinical presentation and the intracellular persistence of the pathogen, Q fever endocarditis often requires a high index of suspicion for timely diagnosis and management.
Understanding Coxiella burnetii and Its Role in Endocarditis
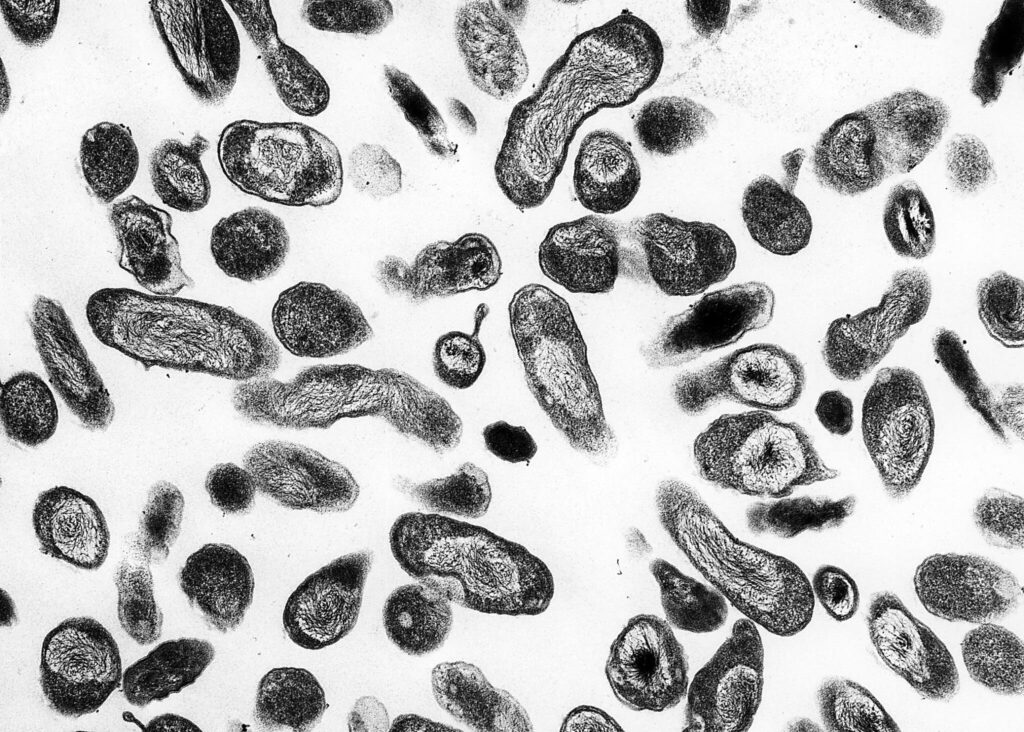
Coxiella burnetii is a gram-negative, obligate intracellular bacterium known for its resistance to environmental stressors and its ability to cause chronic infections. Its proclivity for endothelial surfaces, particularly damaged or prosthetic heart valves, underpins the pathogenesis of Q fever endocarditis.
Pathophysiology of Q Fever Endocarditis
The progression to endocarditis involves several key stages:
The organism’s ability to survive within macrophages and avoid immune clearance facilitates chronic infection, leading to progressive valve destruction and systemic complications.
Risk Factors for Developing Q Fever Endocarditis
- Pre-existing valvular heart disease (e.g., rheumatic heart disease)
- Presence of prosthetic heart valves
- Congenital heart defects
- Vascular grafts and aneurysms
- Immunosuppressive therapy or immunocompromised states
- Previous episodes of acute Q fever
Clinical Manifestations of Q Fever Endocarditis
Common Symptoms
- Prolonged low-grade fever
- Night sweats
- Weight loss
- Fatigue
- Shortness of breath
- Peripheral edema
Physical Examination Findings
- New or changing heart murmur
- Signs of congestive heart failure
- Splenomegaly (enlarged spleen)
- Peripheral stigmata of endocarditis (less common)
Laboratory and Imaging Clues
- Elevated erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP)
- Anemia of chronic disease
- Thrombocytopenia
- Elevated liver enzymes
Diagnostic Strategies for Q Fever Endocarditis
Timely and accurate diagnosis is critical to prevent irreversible cardiac damage.
Serologic Testing
- Phase I IgG titers: Significantly elevated (≥1:800) in chronic infection.
- Phase II IgG and IgM titers: Used to differentiate acute versus chronic phases.
Molecular Methods
- Polymerase Chain Reaction (PCR): Detects Coxiella burnetii DNA in blood or excised valve tissue.
Imaging Studies
- Transthoracic echocardiography (TTE): Initial evaluation.
- Transesophageal echocardiography (TEE): Higher sensitivity for detecting vegetations, prosthetic valve involvement, and abscess formation.
Histopathology and Valve Culture
- Positive findings on valve histopathology with immunohistochemistry are diagnostic.
- Culturing the organism is rarely successful due to its intracellular nature.
Diagnostic Criteria for Q Fever Endocarditis
Modified Duke criteria adapted for Q fever include:
- Positive phase I IgG antibody titer ≥1:800
- Evidence of endocardial involvement by echocardiography
- PCR positivity in blood or tissue samples
- Histologic evidence of infection
Treatment of Q Fever Endocarditis
Antibiotic Therapy
- First-line regimen:
- Doxycycline 100 mg twice daily plus
- Hydroxychloroquine 200 mg three times daily
This combination enhances bacterial clearance by increasing phagolysosomal pH, rendering Coxiella burnetii susceptible to doxycycline.
Duration of Therapy
- Minimum of 18–24 months, often until serologic cure (normalization of phase I IgG titers).
Monitoring
- Regular serologic testing every 3–6 months to assess treatment response.
- Periodic echocardiographic evaluation to monitor valve function.
Surgical Intervention
Indicated in cases of:
- Severe valvular dysfunction
- Large vegetations causing embolization
- Prosthetic valve dehiscence
- Persistent bacteremia despite adequate antimicrobial therapy
Valve replacement is often required to eradicate the infection and restore cardiac function.
Prognosis and Complications
Without appropriate therapy, Q fever endocarditis is almost universally fatal. However, with prompt diagnosis, prolonged antibiotic treatment, and surgical intervention when necessary, survival rates have significantly improved.
Potential Complications
- Heart failure
- Embolic events (e.g., stroke, splenic infarcts)
- Valve perforation
- Systemic immune complex disease
Preventive Measures for High-Risk Individuals
- Early diagnosis and treatment of acute Q fever in patients with predisposing cardiac conditions.
- Prophylactic doxycycline may be considered after high-risk exposures.
- Vaccination (where available) for at-risk populations.
Frequently Asked Questions
How is Q fever endocarditis different from bacterial endocarditis?
Q fever endocarditis is caused by an intracellular organism and typically presents with more indolent symptoms, requires longer antibiotic therapy, and often involves culture-negative blood samples.
Can Q fever endocarditis recur after treatment?
Relapse is possible, especially if antibiotic therapy is prematurely discontinued. Long-term serologic follow-up is critical.
What is the role of hydroxychloroquine in treatment?
Hydroxychloroquine alkalinizes phagolysosomes, thereby enhancing doxycycline’s bactericidal effect against Coxiella burnetii.
Is Q fever endocarditis preventable?
Prompt treatment of acute Q fever and prophylactic measures in high-risk individuals can substantially reduce the risk of chronic infection and endocarditis.
Are there any long-term health effects after successful treatment?
Some patients may experience persistent fatigue or cardiac sequelae requiring ongoing cardiological care.

