Q fever is an acute or chronic zoonotic infection caused by the bacterium Coxiella burnetii. It primarily affects individuals exposed to infected animals, particularly livestock such as cattle, sheep, and goats. The disease can manifest with a wide range of clinical symptoms, from mild flu-like illness to severe complications, including pneumonia, hepatitis, and endocarditis.

Understanding Coxiella burnetii: The Causative Agent
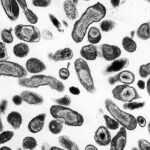
Coxiella burnetii is a highly resilient, gram-negative, obligate intracellular bacterium. It exists in two forms:
- Small-cell variant (SCV): Environmentally resistant, facilitating transmission.
- Large-cell variant (LCV): Metabolically active inside host cells.
The pathogen’s ability to survive in harsh conditions and its airborne transmission route make Q fever a significant public health concern.
Modes of Transmission and Risk Factors
Transmission Routes
- Inhalation of contaminated aerosols: Main transmission pathway.
- Direct contact with infected animals: Especially during birthing processes.
- Consumption of unpasteurized dairy products: Rare but possible.
- Person-to-person transmission: Extremely uncommon.
Risk Factors
- Occupational exposure (veterinarians, farmers, abattoir workers)
- Living near farms or animal facilities
- Immunocompromised status
- Pregnancy (higher risk of severe outcomes)
Clinical Manifestations of Q Fever
Acute Q Fever
Typically presents 2–3 weeks post-exposure.
Common Symptoms
- High-grade fever
- Severe headache
- Myalgia (muscle pain)
- Chills and sweats
- Fatigue
- Cough and chest pain (in cases of pneumonia)
Less Common Symptoms
- Hepatitis with liver function test abnormalities
- Gastrointestinal disturbances
- Rash (rare)
Chronic Q Fever
Occurs in approximately 1–5% of infected individuals, especially those with predisposing conditions.
Clinical Features
- Endocarditis (most frequent chronic manifestation)
- Vascular infections (e.g., infected aneurysms)
- Chronic hepatitis
- Osteomyelitis or chronic bone infections
Complications
- Heart valve damage
- Persistent fatigue syndrome
- Miscarriage or stillbirth in pregnant women
Diagnostic Approach for Q Fever
Clinical Suspicion
Early recognition is critical, especially in high-risk individuals with compatible symptoms.
Laboratory Testing
- Serology: Indirect immunofluorescence assay (IFA) is the gold standard.
- Phase II IgG and IgM antibodies indicate acute infection.
- Phase I IgG titers suggest chronic infection.
- Polymerase Chain Reaction (PCR): Detects Coxiella burnetii DNA, useful in early stages.
- Blood cultures: Rarely positive due to intracellular nature.
- Echocardiography: Recommended for suspected chronic Q fever with cardiac involvement.
Diagnostic Criteria
- Serological evidence (rising antibody titers)
- Positive PCR in blood or tissue samples
- Histopathological findings in tissue biopsy
Treatment Strategies for Q Fever
Acute Q Fever Treatment
- First-line therapy: Doxycycline 100 mg orally twice daily for 14 days
- Alternative therapies: For doxycycline intolerance—fluoroquinolones or trimethoprim-sulfamethoxazole
Chronic Q Fever Treatment
- Combination therapy: Doxycycline plus hydroxychloroquine for at least 18–24 months
- Regular serologic monitoring and imaging assessments are essential.
Special Considerations
- Pregnancy: Cotrimoxazole throughout pregnancy to minimize fetal risks.
- Children under 8 years: Doxycycline remains preferred despite general restrictions due to severity.
Prevention and Control of Q Fever
Vaccination
- Q-Vax®: Effective vaccine available in Australia for at-risk populations.
- Pre-vaccination screening: Mandatory to avoid severe hypersensitivity reactions.
Environmental Control Measures
- Proper disposal of animal birth products
- Control of dust and aerosols in animal facilities
- Regular disinfection protocols
Personal Protective Measures
- Use of personal protective equipment (PPE) by high-risk workers
- Avoidance of raw milk and unpasteurized dairy products
Prognosis and Long-Term Outlook
Most patients with acute Q fever recover fully with appropriate antibiotic therapy. Chronic Q fever requires prolonged treatment and carries a higher risk of morbidity, especially if diagnosis is delayed. Lifelong follow-up may be necessary for individuals with endocarditis or vascular involvement.
Frequently Asked Questions
What is the incubation period for Q fever?
The incubation period typically ranges from 2 to 3 weeks post-exposure.
Can Q fever recur after treatment?
Relapse is rare but possible, particularly in individuals with predisposing conditions such as prosthetic heart valves.
How is chronic Q fever different from acute Q fever?
Chronic Q fever involves persistent infection and can result in severe complications like endocarditis, requiring prolonged combination antibiotic therapy.
Is Q fever contagious between humans?
Person-to-person transmission is extremely rare and not considered a major route of spread.
How effective is the Q fever vaccine?
Q-Vax® provides high protection against infection but requires pre-screening to ensure safety.