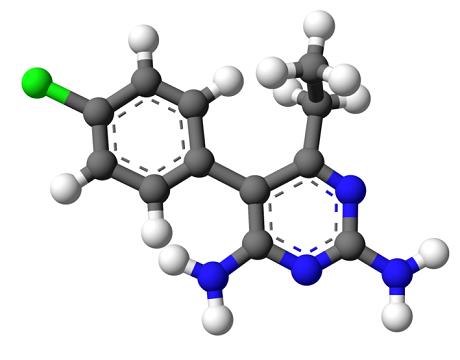
Pyrimethamine is a folic acid antagonist primarily employed in the treatment of protozoal infections such as toxoplasmosis and malaria. By inhibiting dihydrofolate reductase (DHFR), pyrimethamine disrupts DNA synthesis, effectively impairing the replication of parasitic organisms. Despite its therapeutic efficacy, improper dosing or prolonged use can lead to significant toxicity, particularly involving hematologic and neurologic systems.
Mechanism of Pyrimethamine Toxicity
Pyrimethamine’s primary mechanism of toxicity arises from its inhibition of host DHFR, leading to impaired tetrahydrofolate production. This inhibition disrupts nucleotide synthesis, resulting in ineffective hematopoiesis and neurologic dysfunction. The risk of toxicity escalates with high doses, long-term therapy, renal impairment, or concurrent use of other antifolate agents.
Key Pathophysiological Effects
- Bone marrow suppression due to folate depletion
- Neurological impairments from impaired neurotransmitter synthesis
- Gastrointestinal toxicity secondary to mucosal cell turnover inhibition
Causes and Risk Factors of Pyrimethamine Toxicity
Overdose and Dosage Errors
Excessive administration, either acutely or cumulatively, constitutes the primary cause of toxicity. Misinterpretation of dosing regimens, especially in pediatric populations, is a known risk.
Concomitant Folate Deficiency
Underlying folate deficiency potentiates toxicity, increasing the likelihood of severe hematologic complications.
Drug Interactions
- Sulfonamides and other antifolates can enhance toxic effects
- Medications affecting renal clearance may reduce pyrimethamine excretion
Special Populations
- Patients with renal or hepatic impairment
- Pregnant women
- Immunocompromised individuals (e.g., HIV/AIDS patients receiving toxoplasmosis prophylaxis)
Clinical Manifestations of Pyrimethamine Toxicity
Hematologic Symptoms
- Megaloblastic anemia
- Leukopenia
- Thrombocytopenia
- Pancytopenia
Neurological Symptoms
- Headache
- Seizures
- Confusion
- Peripheral neuropathy
Gastrointestinal Symptoms
- Nausea
- Vomiting
- Anorexia
- Abdominal pain
Dermatological Reactions
- Rash
- Stevens-Johnson syndrome (rare, severe)
Other Severe Complications
- Hepatotoxicity
- Renal dysfunction
Diagnostic Approach to Pyrimethamine Toxicity
Clinical Evaluation
Careful history taking regarding drug intake, symptom onset, and associated medications is crucial.
Laboratory Investigations
- Complete Blood Count (CBC): To assess anemia, leukopenia, and thrombocytopenia
- Serum Folate Levels: Typically decreased
- Liver and Renal Function Tests: To monitor organ involvement
- Pyrimethamine Blood Levels: Rarely performed but may confirm overdose
Management of Pyrimethamine Toxicity
Immediate Interventions
- Discontinuation of Pyrimethamine: Primary and most critical step
- Supportive Care: Includes fluid management, monitoring of vital signs, and symptomatic treatment
Folinic Acid (Leucovorin) Rescue Therapy
- Mechanism: Bypasses DHFR blockade by directly providing reduced folate
- Dosing: 5-20 mg of leucovorin IV or orally every 6-8 hours until hematologic recovery
Hematologic Support
- Blood transfusions for severe anemia
- Platelet transfusions if significant thrombocytopenia is present
Management of Severe Cases
- Intensive care monitoring for severe hematologic or neurologic manifestations
- Seizure control with appropriate antiepileptic drugs
Prevention Strategies for Pyrimethamine Toxicity
Proper Dosing and Monitoring
Strict adherence to recommended dosing protocols minimizes toxicity risk.
Folinic Acid Supplementation
Routine co-administration of folinic acid during pyrimethamine therapy is strongly recommended, particularly for patients requiring long-term treatment.
Patient Education
Ensuring patients and caregivers understand dosing instructions and recognize early toxicity signs promotes timely medical intervention.
Regular Laboratory Monitoring
Scheduled CBC, folate, and organ function tests during therapy facilitate early detection of adverse effects.
Prognosis After Pyrimethamine Toxicity
The prognosis is favorable with early recognition and appropriate management. Most patients recover without lasting sequelae if treatment is initiated promptly. However, delayed intervention in cases of severe pancytopenia or neurological involvement can result in permanent complications or, rarely, fatality.
Frequently Asked Questions
What are the early signs of pyrimethamine toxicity?
Early signs include fatigue, pallor, gastrointestinal upset, and easy bruising due to early bone marrow suppression.
How is pyrimethamine toxicity treated?
Immediate drug discontinuation, folinic acid rescue, and supportive care form the cornerstone of management.
Can pyrimethamine toxicity be fatal?
Although rare, untreated severe toxicity can lead to fatal pancytopenia or multi-organ failure.
How long does recovery from pyrimethamine toxicity take?
Recovery time varies but typically spans days to weeks, depending on the severity of toxicity and timely initiation of treatment.
Should folic acid or folinic acid be used with pyrimethamine?
Folinic acid (leucovorin), not folic acid, is preferred as it bypasses the inhibited DHFR enzyme.