Acute decompensated heart failure (ADHF) is a critical condition requiring prompt diagnosis and intervention. Characterized by a sudden or gradual worsening of heart failure symptoms, ADHF often leads to hospitalizations and can result in severe complications if left untreated. This article explores the causes, clinical presentation, diagnostic methods, and management strategies to optimize patient outcomes.
What Is Acute Decompensated Heart Failure?
Acute decompensated heart failure is defined as a rapid onset or progression of heart failure symptoms, typically manifesting as fluid overload, dyspnea, and impaired organ perfusion. It is a leading cause of hospital admissions worldwide, particularly in older adults with underlying chronic heart failure.
Key Features of ADHF
- Fluid Overload: The most common symptom, leading to pulmonary congestion and peripheral edema.
- Elevated Left Ventricular Filling Pressure: Impairs cardiac output and contributes to symptoms like fatigue and breathlessness.
- Systemic Hypoperfusion: Can result in organ dysfunction, including renal impairment and altered mental status.
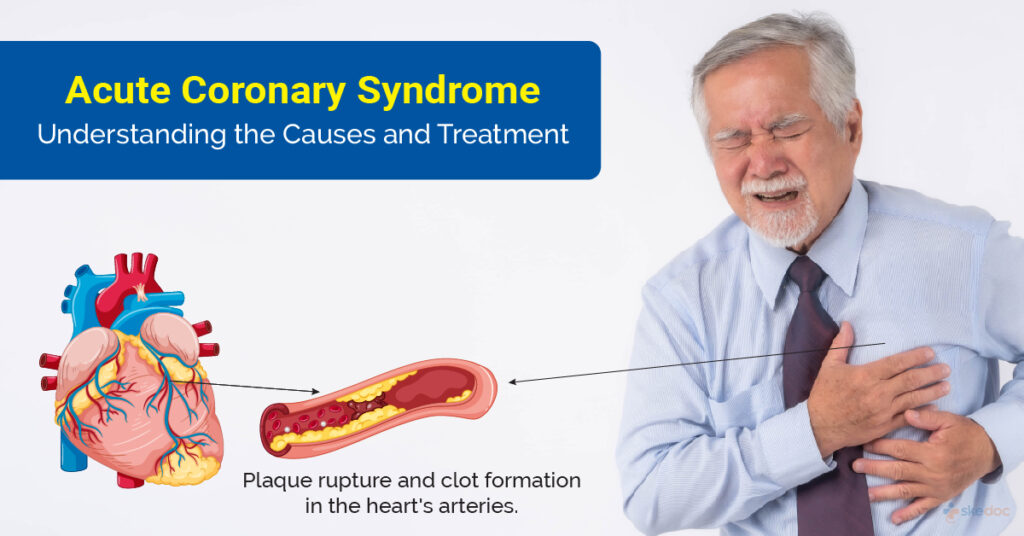
Causes and Risk Factors of ADHF
ADHF often results from precipitating factors that exacerbate existing heart failure or overwhelm cardiac compensatory mechanisms. Common causes and risk factors include:
- Noncompliance with Medications or Diet: High sodium intake or missed doses of diuretics can trigger fluid retention.
- Cardiac Events: Acute myocardial infarction, arrhythmias, or valvular dysfunction can lead to sudden decompensation.
- Infections: Pulmonary infections or sepsis can increase metabolic demands, worsening heart failure.
- Uncontrolled Hypertension: Elevated blood pressure increases afterload, reducing cardiac output.
- Renal Dysfunction: Impaired renal function exacerbates fluid retention and electrolyte imbalances.
- Medications: Certain drugs, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or negative inotropes, may precipitate ADHF.
Clinical Presentation of ADHF
Patients with ADHF present with a range of symptoms and signs depending on the severity of the condition. These may include:
Symptoms
- Dyspnea: Ranging from exertional to severe orthopnea or paroxysmal nocturnal dyspnea.
- Fatigue and Weakness: Due to reduced cardiac output and systemic hypoperfusion.
- Chest Pain: Particularly if the underlying cause is ischemic in nature.
Signs
- Pulmonary Rales: Indicating fluid accumulation in the lungs.
- Peripheral Edema: Seen in lower extremities or sacral regions.
- Jugular Venous Distension: Suggesting elevated right-sided filling pressures.
- Tachycardia and Hypotension: Indicating compensatory mechanisms or systemic hypoperfusion.
Diagnostic Approach to Acute Decompensated Heart Failure
Prompt diagnosis of ADHF is critical to initiate appropriate treatment. A structured approach combining clinical evaluation, imaging, and laboratory testing is essential.
1. Clinical Assessment
- Detailed history of symptoms, onset, and triggers.
- Physical examination to evaluate fluid status and perfusion.
2. Imaging Studies
- Chest X-Ray: Reveals pulmonary congestion or cardiomegaly.
- Echocardiography: Assesses left ventricular function, valvular abnormalities, and ejection fraction.
3. Laboratory Testing
- BNP/NT-proBNP Levels: Elevated levels indicate heart failure and help differentiate ADHF from other causes of dyspnea.
- Renal Function Tests: Assess renal perfusion and electrolyte status.
- Arterial Blood Gases (ABG): Evaluate oxygenation and acid-base status.
4. Hemodynamic Monitoring
Invasive monitoring with pulmonary artery catheters may be used in critically ill patients to guide therapy.
Management Strategies for Acute Decompensated Heart Failure
Treatment of ADHF focuses on relieving symptoms, optimizing hemodynamics, and addressing underlying causes. Key components of management include:
1. Oxygen Therapy
Administer oxygen to alleviate hypoxia, with noninvasive ventilation or mechanical ventilation in severe cases.
2. Pharmacologic Interventions
Diuretics
- Loop Diuretics: First-line agents to reduce fluid overload. Intravenous administration provides rapid relief.
Vasodilators
- Nitroglycerin or Nitroprusside: Reduces preload and afterload, improving symptoms of congestion.
Inotropes
- Dobutamine or Milrinone: Used in patients with low cardiac output and evidence of hypoperfusion.
Vasopressors
- Norepinephrine: May be required in cases of severe hypotension and shock.
3. Non-Pharmacologic Measures
- Fluid Restriction: Essential in patients with significant fluid overload.
- Sodium Restriction: Prevents further fluid retention.
- Close Monitoring: Frequent assessment of weight, fluid status, and hemodynamics is critical.
Long-Term Management and Prevention
Once stabilized, patients with ADHF require a structured discharge plan to prevent rehospitalizations.
1. Medication Optimization
Ensure adherence to guideline-directed medical therapy, including beta-blockers, ACE inhibitors, ARBs, or ARNI.
2. Lifestyle Modifications
- Sodium restriction (<2g/day) and fluid restriction as advised.
- Regular physical activity and weight monitoring.
3. Follow-Up and Education
Frequent outpatient follow-ups to assess symptoms and medication efficacy are crucial. Patient education on recognizing early signs of decompensation is vital.
Acute decompensated heart failure is a complex and life-threatening condition that demands immediate and comprehensive intervention. By understanding its causes, clinical presentation, and treatment options, healthcare professionals can effectively manage ADHF and reduce its associated morbidity and mortality.