Pyelonephritis is a serious bacterial infection affecting one or both kidneys, often originating from a urinary tract infection (UTI) that has spread upwards. If untreated, it can cause irreversible kidney damage or life-threatening complications. Prompt diagnosis and appropriate management are critical to preserving renal function and overall health.
Types of Pyelonephritis
Acute Pyelonephritis
Acute pyelonephritis is a sudden and severe kidney infection characterized by rapid onset of symptoms, including fever, flank pain, and urinary disturbances. It requires urgent antibiotic therapy to prevent systemic spread of infection.
Chronic Pyelonephritis
Chronic pyelonephritis results from recurrent infections or persistent inflammation, leading to progressive renal scarring, functional impairment, and ultimately, chronic kidney disease if not addressed.
Symptoms of Pyelonephritis
- High fever and chills
- Pain in the back, side, or groin
- Frequent, painful urination
- Cloudy or foul-smelling urine
- Nausea and vomiting
- Fatigue and malaise
- Hematuria (blood in urine)
- Confusion in elderly patients
Severe cases may present with signs of sepsis, requiring immediate hospitalization.
Causes and Risk Factors
Several factors can predispose individuals to pyelonephritis:
- Urinary tract infections (UTIs): Most common cause, especially when caused by Escherichia coli bacteria.
- Urinary obstruction: Kidney stones, tumors, or structural abnormalities can block urine flow.
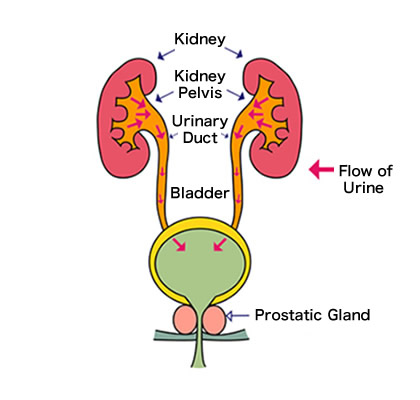
- Vesicoureteral reflux: A congenital condition where urine flows backward from the bladder toward the kidneys.
- Catheter use: Indwelling urinary catheters increase infection risk.
- Diabetes mellitus: Elevated blood sugar levels can impair immune defenses.
- Pregnancy: Hormonal and anatomical changes increase susceptibility.
- Immunosuppression: Weakened immune systems from medications or diseases elevate infection risk.
Diagnosis of Pyelonephritis
Accurate diagnosis is essential for effective treatment and prevention of complications. Diagnostic methods include:
- Urinalysis: Detects white blood cells, bacteria, and blood in urine.
- Urine culture: Identifies the specific bacteria causing the infection.
- Blood cultures: Necessary in suspected cases of sepsis.
- Imaging studies:
- Ultrasound: Useful for detecting obstructions or abscesses.
- CT scan: Provides detailed visualization of renal structures, preferred in complicated cases.
Prompt and precise diagnosis guides the selection of appropriate therapy and the prevention of long-term damage.
Treatment Options for Pyelonephritis
Antibiotic Therapy
- Empiric antibiotics: Initiated immediately after diagnosis, typically targeting gram-negative bacteria.
- Tailored therapy: Adjusted based on urine culture results.
- Intravenous antibiotics: Required for severe infections or hospitalized patients.
- Oral antibiotics: Suitable for uncomplicated cases, usually continued for 10–14 days.
Hospitalization
Hospital admission is necessary in the following scenarios:
- Severe illness with high fever, vomiting, or dehydration
- Pregnancy
- Immunocompromised status
- Elderly patients with cognitive impairment
Surgical Intervention
Surgical procedures may be required to correct underlying anatomical abnormalities, drain abscesses, or remove obstructions such as stones.
Supportive Measures
- Adequate hydration to flush bacteria from the urinary tract
- Pain management using analgesics
- Monitoring for signs of systemic infection
Prevention Strategies
Effective prevention reduces the risk of recurrent pyelonephritis:
- Early treatment of urinary tract infections
- Proper hygiene practices
- Adequate fluid intake
- Regular voiding habits: Avoid holding urine for prolonged periods
- Management of underlying conditions: Such as diabetes and urinary tract abnormalities
In recurrent cases, prophylactic low-dose antibiotics may be recommended under medical supervision.
Frequently Asked Questions
What are the early warning signs of pyelonephritis?
Early signs include high fever, flank or back pain, frequent and painful urination, and nausea.
Can pyelonephritis resolve without treatment?
No, untreated pyelonephritis can lead to serious complications, including kidney damage, sepsis, and death.
How is pyelonephritis different from a regular UTI?
A regular UTI affects the bladder and urethra, whereas pyelonephritis involves the kidneys and is more severe, requiring aggressive treatment.
What is the best antibiotic for pyelonephritis?
Empirical choices often include fluoroquinolones, third-generation cephalosporins, or aminoglycosides, tailored based on bacterial culture results.
Is hospitalization always required for pyelonephritis?
Not always; mild cases can be treated with oral antibiotics at home. However, severe, complicated, or high-risk cases need inpatient care.

