Pustular psoriasis is a rare and severe form of psoriasis characterized by the presence of white, pus-filled blisters (pustules) surrounded by red, inflamed skin. Unlike infections, the pus consists of non-infectious white blood cells. Pustular psoriasis may occur on localized areas, such as the hands and feet, or it can affect the entire body, leading to life-threatening complications if untreated.

Types of Pustular Psoriasis
Generalized Pustular Psoriasis (GPP)
Generalized pustular psoriasis (GPP) is an acute and severe form of pustular psoriasis that affects large areas of the body. It is marked by widespread redness, pustules, fever, chills, and fatigue. GPP is considered a medical emergency requiring immediate intervention.
Palmoplantar Pustulosis (PPP)
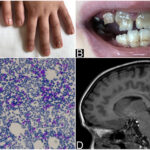
Palmoplantar pustulosis (PPP) affects the palms of the hands and the soles of the feet. It is characterized by recurring pustules that may lead to painful cracks and scaling.
Acrodermatitis Continua of Hallopeau (ACH)
Acrodermatitis continua of Hallopeau (ACH) primarily involves the fingertips and toes. It often leads to nail changes, chronic inflammation, and sometimes bone involvement if left untreated.
Symptoms of Pustular Psoriasis
- Formation of painful pustules
- Red, tender, and swollen skin
- Scaling and flaking of affected areas
- Systemic symptoms such as fever, chills, and fatigue
- Itching and burning sensations
- Nausea and rapid heart rate in severe cases
The symptoms may vary based on the specific type and severity of the condition.
Causes and Risk Factors
The exact cause of pustular psoriasis remains unclear, but several factors are known to trigger or exacerbate the condition:
- Genetic predisposition: Mutations in the IL36RN gene are linked to GPP.
- Withdrawal from systemic corticosteroids
- Infections: Viral or bacterial infections may trigger outbreaks.
- Stress: Psychological stress can precipitate flare-ups.
- Pregnancy: Impetigo herpetiformis, a variant of pustular psoriasis, can occur during pregnancy.
- Certain medications: Such as lithium, antimalarials, or beta-blockers.
- Environmental factors: Smoking and exposure to certain chemicals.
Diagnosis of Pustular Psoriasis
Diagnosis is primarily clinical, involving a detailed medical history and physical examination. Dermatologists may perform the following tests to confirm the diagnosis:
- Skin biopsy: A small sample of affected skin examined under a microscope.
- Blood tests: To detect signs of infection, inflammation, and electrolyte imbalances.
- Imaging tests: In severe cases, X-rays or MRI may be required to check joint or bone involvement.
Treatment Options for Pustular Psoriasis
Topical Therapies
- Corticosteroids: Reduce inflammation and immune response.
- Vitamin D analogs: Help regulate skin cell production.
- Coal tar preparations: Traditional remedy with anti-inflammatory properties.
Systemic Treatments
- Retinoids: Such as acitretin, effective for generalized pustular psoriasis.
- Methotrexate: Immunosuppressant used to control severe symptoms.
- Cyclosporine: Rapid action for critical cases.
- Biologic agents: TNF-alpha inhibitors (e.g., infliximab, adalimumab) and IL-17 inhibitors (e.g., secukinumab) target specific immune pathways.
Emerging Treatments
Newer biologics targeting IL-36 pathways, such as spesolimab, show promising results in treating GPP flares.
Supportive Care
- Hospitalization: In severe cases to manage fluids, infections, and vital signs.
- Wound care: Specialized dressings to protect skin integrity.
- Pain management: Analgesics to control discomfort.
Managing and Preventing Flare-Ups
- Adherence to treatment plans: Strictly following prescribed therapies.
- Avoidance of known triggers: Such as stress, smoking, and certain medications.
- Regular dermatological check-ups: Early intervention helps prevent severe complications.
- Healthy lifestyle: A balanced diet, hydration, and stress-reduction techniques contribute to overall skin health.
Complications Associated with Pustular Psoriasis
If left untreated, pustular psoriasis can lead to:
- Sepsis
- Heart failure
- Electrolyte imbalances
- Liver and kidney complications
- Psychological distress due to visible skin changes
Early and aggressive treatment is crucial to prevent these potentially life-threatening complications.
Frequently Asked Questions
What is the main cause of pustular psoriasis?
While the exact cause is unknown, genetic mutations, immune system dysfunctions, and environmental triggers are major contributors.
Is pustular psoriasis contagious?
No, pustular psoriasis is not contagious. It results from immune system dysfunction, not infection.
Can pustular psoriasis be cured?
There is no permanent cure, but with proper management, individuals can achieve long-term remission and improved quality of life.
What is the most severe form of pustular psoriasis?
Generalized pustular psoriasis (GPP) is considered the most severe form, often requiring immediate hospitalization.
Which medications are best for treating pustular psoriasis?
Treatment varies by severity but commonly includes retinoids, methotrexate, cyclosporine, and targeted biologic therapies like IL-17 or IL-36 inhibitors.