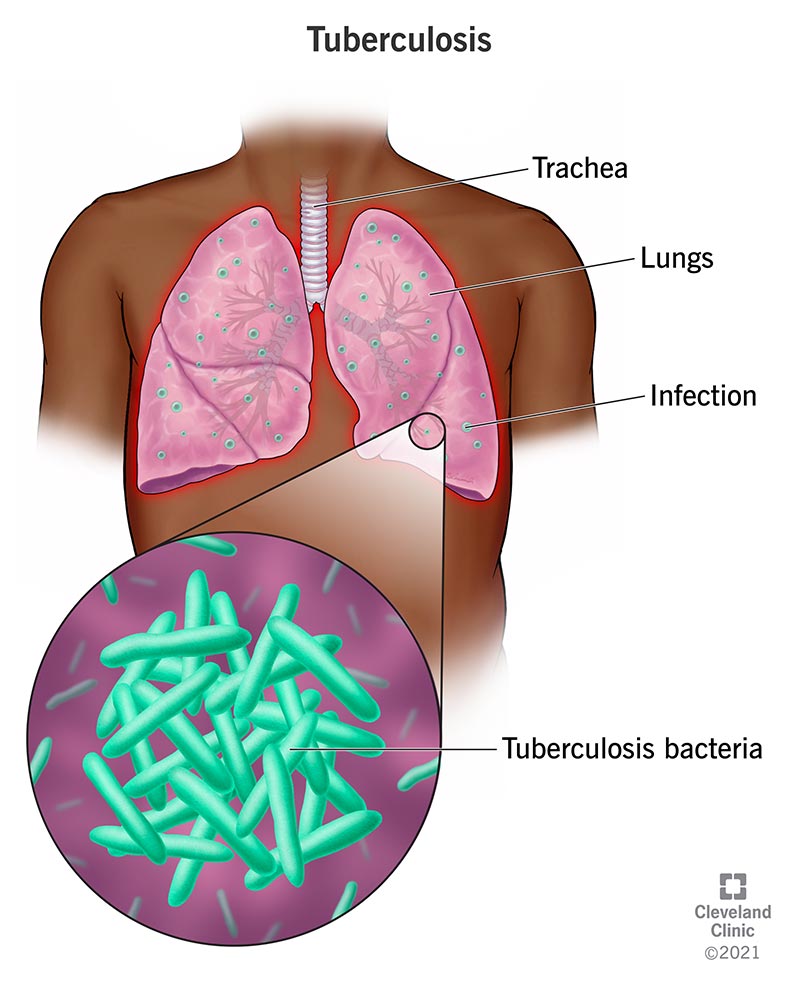
Pulmonary tuberculosis (TB) is a contagious and potentially life-threatening infection caused primarily by Mycobacterium tuberculosis. It most commonly affects the lungs but can spread to other organs through the bloodstream or lymphatic system. Despite global efforts to eliminate TB, it remains a major public health challenge, particularly in low- and middle-income countries.
Etiology: Understanding the Causative Agent
Mycobacterium tuberculosis is a slow-growing, acid-fast bacillus transmitted from person to person through airborne particles. Once inhaled, the bacteria may be eliminated by the immune system or remain dormant, leading to latent TB infection (LTBI), which can reactivate and develop into active disease under immunocompromised conditions.
Pathogenesis: How Pulmonary TB Develops
Following inhalation, TB bacilli reach the alveoli where they are engulfed by alveolar macrophages. In some cases, the bacteria survive and replicate, leading to the formation of granulomas—organized immune cell clusters attempting to contain the infection. If the immune system fails, bacilli multiply and spread, causing pulmonary damage.
Clinical Manifestations of Pulmonary Tuberculosis
The symptoms of pulmonary TB are often insidious but progressively worsen without treatment. Common clinical features include:
- Persistent cough lasting more than 2–3 weeks
- Hemoptysis (coughing up blood)
- Chest pain
- Fever and night sweats
- Unexplained weight loss
- Fatigue and malaise
In advanced cases, pulmonary function deteriorates due to cavitary lesions and fibrosis, increasing the risk of respiratory failure.
Diagnostic Approaches for Pulmonary TB
Accurate and early diagnosis of TB is critical for controlling transmission and initiating treatment.
Microbiological Testing
- Sputum smear microscopy: Detects acid-fast bacilli (AFB); widely used in resource-limited settings
- Culture: Gold standard for TB diagnosis; enables drug susceptibility testing
- Nucleic acid amplification tests (NAATs): Provide rapid detection and rifampicin resistance results
Radiographic Evaluation
- Chest X-ray: Reveals characteristic lesions such as upper lobe infiltrates, cavitation, and fibrosis
- CT Scan: Offers detailed imaging, especially in complex or atypical cases
Immunological Tests
- Tuberculin skin test (TST): Indicates exposure to TB but cannot distinguish active from latent infection
- Interferon-gamma release assays (IGRAs): More specific, especially in BCG-vaccinated individuals
Treatment Protocols for Pulmonary Tuberculosis
Standard treatment regimens are designed to eliminate the bacilli and prevent drug resistance.
First-Line Anti-TB Drugs
- Isoniazid (H)
- Rifampicin (R)
- Pyrazinamide (Z)
- Ethambutol (E)
The intensive phase lasts for two months (HRZE), followed by a continuation phase of four months (HR).
Directly Observed Treatment, Short-course (DOTS)
WHO recommends DOTS to ensure adherence, reduce drug resistance, and enhance treatment outcomes. Under DOTS, healthcare workers observe patients taking their medications daily.
Management of Drug-Resistant TB
Multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB) require prolonged treatment with second-line agents such as:
- Fluoroquinolones (e.g., levofloxacin, moxifloxacin)
- Injectable agents (e.g., amikacin, capreomycin)
- Bedaquiline and delamanid (for resistant strains)
Prevention and Control Measures
Preventing TB transmission is crucial to global health efforts. Strategies include:
Vaccination
- BCG vaccine: Offers protection in children against severe TB forms, although efficacy in adults is variable.
Infection Control in Healthcare Settings
- Use of personal protective equipment (PPE)
- Ventilation and ultraviolet germicidal irradiation (UVGI)
- Prompt isolation of infectious patients
Community-Based Interventions
- Contact tracing and screening
- Public education and awareness campaigns
- Strengthening primary care and TB surveillance systems
TB in High-Risk Populations
Certain groups are more vulnerable to TB and require targeted interventions.
HIV Co-Infection
TB is a leading cause of mortality in people with HIV. Integration of TB and HIV services, prophylaxis with isoniazid, and antiretroviral therapy (ART) are vital.
Diabetes Mellitus
Impaired immunity in diabetic individuals increases susceptibility to TB. Glycemic control enhances treatment outcomes.
Children and the Elderly
Both age groups may present with atypical symptoms and require modified diagnostic and therapeutic approaches.
Global Epidemiology and Public Health Response
According to the World Health Organization, pulmonary TB remains one of the top 10 causes of death globally. Efforts under the End TB Strategy aim to reduce TB deaths by 90% and incidence by 80% by 2030.
Key Global Strategies
- Expanding access to diagnostic tools and treatment
- Investment in vaccine development and TB research
- Multisectoral collaboration and patient-centered care
Pulmonary tuberculosis is a persistent global health threat, yet it is curable and preventable through early diagnosis, effective treatment, and robust public health strategies. A unified effort encompassing clinical excellence, community awareness, and global policy enforcement is essential to eradicate this ancient disease.