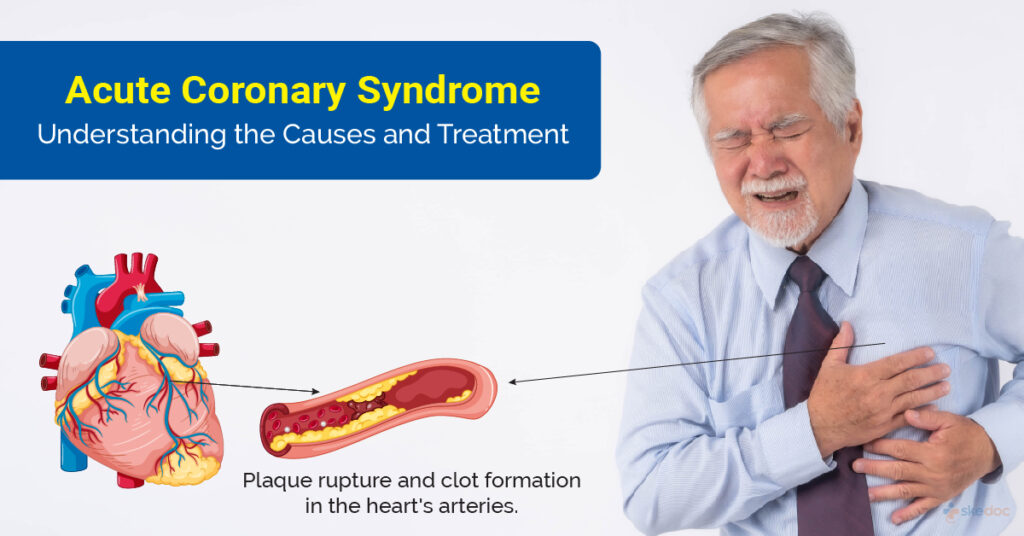
Acute coronary syndrome (ACS) is a critical medical condition resulting from sudden, reduced blood flow to the heart. This condition encompasses a spectrum of disorders, including unstable angina and myocardial infarction (heart attack). Early diagnosis and prompt treatment are essential to prevent life-threatening complications. In this comprehensive guide, we explore the causes, symptoms, diagnostic methods, and treatment strategies for ACS, providing a detailed resource for healthcare professionals and patients alike.
Understanding Acute Coronary Syndrome
Acute coronary syndrome refers to a group of conditions caused by a significant reduction or blockage of blood supply to the heart muscle. The underlying mechanism typically involves the rupture of an atherosclerotic plaque within a coronary artery, leading to the formation of a blood clot (thrombus). The severity and duration of blood flow reduction determine the clinical manifestation, ranging from unstable angina to non-ST-segment elevation myocardial infarction (NSTEMI) and ST-segment elevation myocardial infarction (STEMI).
Causes and Risk Factors
Several factors contribute to the development of ACS. Key causes and risk factors include:
- Atherosclerosis: The most common cause of ACS, involving the buildup of fatty deposits (plaques) in coronary arteries.
- Thrombosis: Formation of a blood clot at the site of a ruptured plaque.
- Spasms of Coronary Arteries: Sudden constriction of coronary arteries, reducing blood flow.
- Age: Risk increases with age, particularly in men over 45 and women over 55.
- Lifestyle Factors: Smoking, high-fat diets, lack of physical activity, and excessive alcohol consumption.
- Medical Conditions: Hypertension, diabetes, obesity, and high cholesterol levels.
- Family History: Genetic predisposition to heart disease.
Recognizing Symptoms of Acute Coronary Syndrome
Symptoms of ACS can vary depending on the severity and type of condition. Common symptoms include:
- Chest pain or discomfort, often described as a tightness, pressure, or burning sensation.
- Pain radiating to the shoulders, arms, back, neck, or jaw.
- Shortness of breath or difficulty breathing.
- Sweating (diaphoresis), nausea, or lightheadedness.
- Fatigue, particularly in women and older adults.
It is important to note that some patients, particularly those with diabetes, may experience atypical or less pronounced symptoms, making diagnosis more challenging.
Diagnosis of Acute Coronary Syndrome
Accurate diagnosis of ACS involves a combination of clinical assessment, laboratory tests, and imaging studies. Common diagnostic methods include:
1. Electrocardiogram (ECG)
The ECG is a primary tool for diagnosing ACS. It helps identify changes in heart electrical activity, distinguishing between STEMI, NSTEMI, and unstable angina.
2. Blood Tests
Measurement of cardiac biomarkers, such as troponin levels, is critical in detecting myocardial injury. Elevated troponin levels confirm the presence of a heart attack.
3. Imaging Studies
- Coronary Angiography: Identifies blockages or narrowing in coronary arteries.
- Echocardiography: Assesses heart function and detects complications such as valve dysfunction or heart failure.
4. Clinical Evaluation
A thorough history and physical examination are essential to identify risk factors and evaluate the patient’s overall condition.
Treatment Strategies for Acute Coronary Syndrome
The management of ACS aims to restore blood flow to the heart, prevent further complications, and improve long-term outcomes. Treatment typically involves a combination of medications, invasive procedures, and lifestyle changes.
1. Medications
- Antiplatelet Agents: Aspirin and P2Y12 inhibitors (e.g., clopidogrel) reduce the risk of clot formation.
- Anticoagulants: Heparin or direct oral anticoagulants (DOACs) prevent clot extension.
- Nitroglycerin: Relieves chest pain by dilating coronary arteries.
- Beta-Blockers: Reduce heart workload and prevent arrhythmias.
- Statins: Lower cholesterol levels and stabilize plaques.
2. Revascularization Procedures
- Percutaneous Coronary Intervention (PCI): A minimally invasive procedure involving the placement of a stent to open blocked arteries.
- Coronary Artery Bypass Grafting (CABG): Surgical rerouting of blood flow around blocked arteries.
3. Long-Term Management
- Lifestyle Modifications: Smoking cessation, regular exercise, a heart-healthy diet, and stress management.
- Cardiac Rehabilitation: A structured program to improve cardiovascular health and reduce recurrence risk.
Preventing Acute Coronary Syndrome
Prevention of ACS involves addressing modifiable risk factors and adopting healthy habits. Strategies include:
- Regular Health Screenings: Monitor blood pressure, cholesterol, and glucose levels.
- Heart-Healthy Diet: Incorporate whole grains, lean proteins, fruits, and vegetables.
- Exercise: Engage in at least 150 minutes of moderate aerobic activity weekly.
- Weight Management: Maintain a healthy body weight.
- Smoking Cessation: Avoid tobacco use in all forms.
Acute coronary syndrome represents a significant challenge in modern medicine due to its high prevalence and potential for severe complications. Early recognition, prompt treatment, and long-term management are vital for improving survival rates and quality of life for patients. By addressing modifiable risk factors and implementing evidence-based prevention strategies, healthcare providers and patients can work together to reduce the burden of ACS.