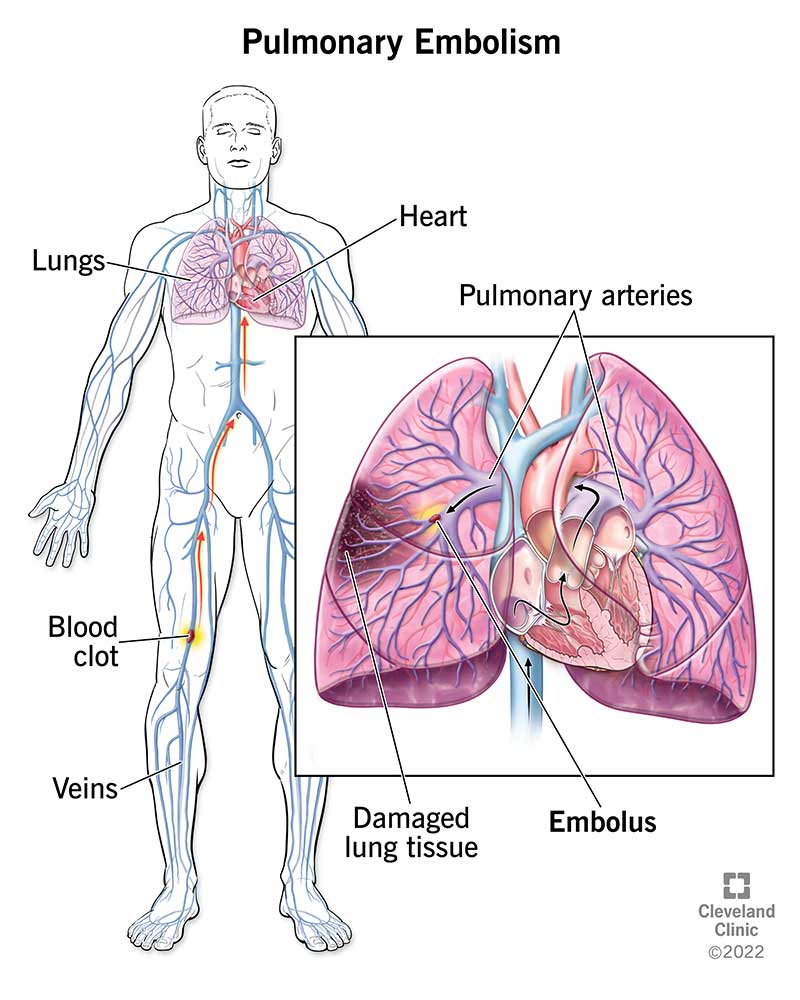
Pulmonary thromboembolism (PTE), commonly referred to as pulmonary embolism, is a potentially life-threatening condition caused by the obstruction of the pulmonary arteries by thrombi, typically originating from deep veins in the lower extremities. It constitutes a major component of venous thromboembolism (VTE), alongside deep vein thrombosis (DVT). The prompt recognition and treatment of PTE are essential to reduce morbidity and mortality.
Pathophysiology of Pulmonary Embolism
A thrombus formed in the deep veins of the legs or pelvis may dislodge and travel through the venous system, reaching the right heart and subsequently the pulmonary arteries. Once lodged in the pulmonary vasculature, the embolus disrupts normal blood flow, causing ventilation-perfusion mismatch, increased pulmonary vascular resistance, and right ventricular strain.
Hemodynamic Consequences
- Increased pulmonary artery pressure
- Decreased cardiac output due to right ventricular dysfunction
- Potential cardiogenic shock in massive embolism
Classification of Pulmonary Embolism
- Massive PE: Causes hypotension or cardiac arrest
- Submassive PE: No hypotension but with right ventricular dysfunction
- Low-risk PE: Hemodynamically stable without RV dysfunction
Risk Factors for Pulmonary Thromboembolism
Several clinical and acquired factors increase the likelihood of thromboembolic events:
Acquired Risk Factors
- Prolonged immobilization
- Recent surgery, especially orthopedic
- Malignancy
- Pregnancy and postpartum state
- Estrogen therapy or oral contraceptives
- Obesity
- Smoking
Inherited Risk Factors
- Factor V Leiden mutation
- Prothrombin gene mutation
- Protein C, Protein S, or Antithrombin III deficiency
Clinical Presentation and Symptoms
Pulmonary thromboembolism presents with a wide spectrum of symptoms, often making diagnosis challenging. Classic features include:
- Sudden onset dyspnea
- Pleuritic chest pain
- Tachypnea and tachycardia
- Hemoptysis (less common)
- Syncope in massive PE
- Signs of DVT: unilateral leg swelling, tenderness
In many cases, symptoms may be nonspecific, especially in elderly or comorbid patients.
Diagnostic Approach to Pulmonary Thromboembolism
Accurate and timely diagnosis is crucial to initiate life-saving therapy. The evaluation includes clinical probability assessment, imaging, and laboratory investigations.
1. Clinical Risk Stratification
- Wells Score or Geneva Score to estimate pretest probability
- Categorization: Low, Intermediate, or High clinical suspicion
2. D-Dimer Testing
- High sensitivity for ruling out PE in low-risk patients
- Not specific and may be elevated in infection, malignancy, or pregnancy
3. Imaging Modalities
- CT Pulmonary Angiography (CTPA): Gold standard; directly visualizes emboli in pulmonary arteries
- Ventilation-Perfusion (V/Q) Scan: Used in patients with contrast allergy or renal impairment
- Echocardiography: Useful in detecting right ventricular strain in massive PE
4. Additional Tests
- Lower limb Doppler ultrasound for DVT confirmation
- Arterial blood gases: Hypoxemia and hypocapnia in PE
- ECG: Sinus tachycardia, S1Q3T3 pattern in severe cases
Management of Pulmonary Thromboembolism
Treatment aims to prevent further thrombus propagation, facilitate clot resolution, and reduce long-term complications.
1. Initial Stabilization
- Oxygen therapy
- Intravenous fluids for hypotension
- Vasopressors for shock (norepinephrine preferred)
2. Anticoagulation Therapy
- Low Molecular Weight Heparin (LMWH) or Unfractionated Heparin
- Transition to oral anticoagulants such as:
- Vitamin K antagonists (e.g., warfarin)
- Direct oral anticoagulants (DOACs): rivaroxaban, apixaban, dabigatran
3. Thrombolytic Therapy
- Indicated in massive PE with hemodynamic instability
- Agents: Alteplase (tPA)
- Contraindications must be carefully assessed (e.g., recent surgery, bleeding risk)
4. Surgical or Catheter-Based Interventions
- Embolectomy: For patients who cannot receive thrombolysis
- Catheter-directed thrombolysis or fragmentation in selected cases
5. Inferior Vena Cava (IVC) Filters
- Considered in patients with contraindications to anticoagulation or recurrent PE despite adequate therapy
Long-Term Management and Secondary Prevention
Patients with PE require prolonged anticoagulation to prevent recurrence and manage underlying prothrombotic states.
Duration of Anticoagulation
- 3 months: Provoked PE with transient risk factor
- 6–12 months or lifelong: Unprovoked PE or persistent risk factors
Follow-up
- Monitor for post-PE syndrome and chronic thromboembolic pulmonary hypertension (CTEPH)
- Evaluate bleeding risks regularly during anticoagulant use
Complications of Pulmonary Thromboembolism
If inadequately treated, PE can lead to significant complications:
- Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
- Right heart failure
- Recurrent venous thromboembolism
- Post-thrombotic syndrome
Prevention Strategies for Pulmonary Thromboembolism
Effective prevention is a cornerstone of reducing incidence, especially in high-risk patients.
Mechanical Prophylaxis
- Graduated compression stockings
- Intermittent pneumatic compression devices
Pharmacologic Prophylaxis
- LMWH or fondaparinux post-operatively
- Dose adjustments based on renal function and bleeding risk
Pulmonary thromboembolism remains a significant clinical challenge requiring a high index of suspicion, rapid diagnostic evaluation, and evidence-based management. With improved diagnostic algorithms, risk stratification tools, and therapeutic options, outcomes have markedly improved. Continued vigilance and preventive strategies remain essential to reducing the global burden of PTE.