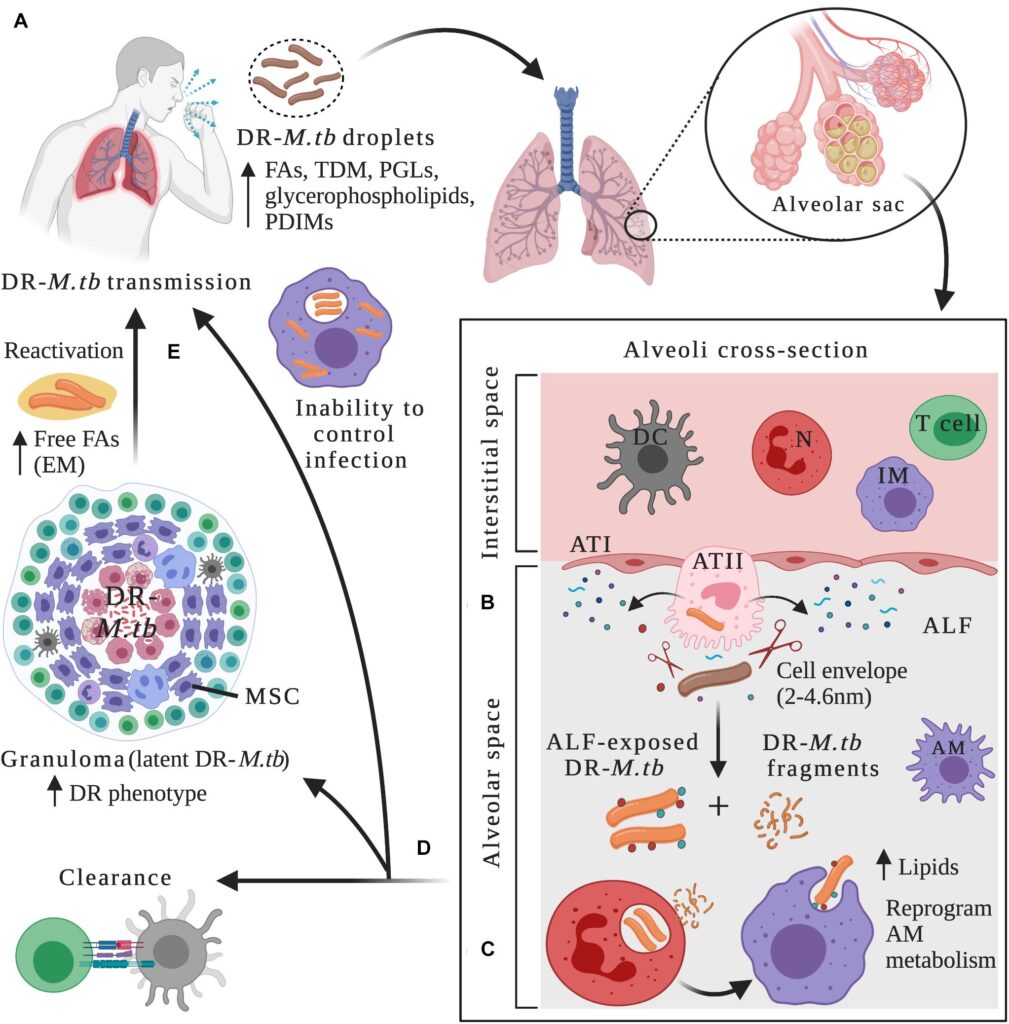
Pulmonary multi-drug resistant Mycobacterium tuberculosis (MDR-TB) represents a severe and escalating public health crisis, marked by resistance to at least isoniazid and rifampin, the two most potent first-line antitubercular drugs. This resistance complicates treatment, prolongs infectiousness, and elevates mortality rates. The disease primarily affects the lungs, facilitating airborne transmission and making containment efforts challenging in both high-burden and emerging-risk regions.
Etiology and Mechanisms of Drug Resistance in Mycobacterium Tuberculosis
MDR-TB arises through spontaneous genetic mutations within the Mycobacterium tuberculosis genome. When these mutations occur in genes associated with drug targets or metabolism, resistance ensues. Inadequate or interrupted treatment regimens, substandard medications, and poor patient adherence further drive the selection and propagation of resistant strains.
Genetic Mutations Associated with Resistance
- katG and inhA mutations → resistance to isoniazid
- rpoB mutations → resistance to rifampin
- Cross-resistance often accompanies fluoroquinolones and second-line injectables in extensively drug-resistant TB (XDR-TB)
Global Burden and Epidemiological Trends
According to the World Health Organization (WHO), approximately 450,000 new cases of MDR-TB were reported in 2022, with a concentration in India, China, the Russian Federation, and South Africa. Pulmonary MDR-TB disproportionately affects marginalized communities and those with compromised healthcare access.
High-Risk Populations
- Previously treated TB patients
- HIV-infected individuals
- Residents of overcrowded or correctional facilities
- Healthcare workers in TB-endemic areas
Clinical Presentation of Pulmonary MDR-TB
The symptoms of pulmonary MDR-TB closely resemble those of drug-susceptible TB but are often more prolonged and severe due to delayed effective treatment.
Common Symptoms
- Persistent cough lasting more than 3 weeks
- Hemoptysis (coughing up blood)
- Night sweats
- Unexplained weight loss
- Fever and chills
- Dyspnea in advanced stages
Physical examination may reveal crackles over the lungs, clubbing, and signs of cachexia in chronic cases.
Diagnostic Strategy for Pulmonary MDR-TB
Early and accurate diagnosis is crucial to initiate appropriate therapy and interrupt transmission. Diagnosis relies on a combination of clinical suspicion, imaging, and microbiological confirmation.
1. Sputum Microscopy and Culture
- Ziehl-Neelsen staining for acid-fast bacilli (AFB)
- Mycobacterial culture on Löwenstein-Jensen or liquid media for confirmation
2. Molecular Diagnostics
- GeneXpert MTB/RIF: Rapid detection of rifampin resistance
- Line Probe Assay (LPA): Identifies mutations for isoniazid and rifampin resistance
- Whole Genome Sequencing (WGS): Emerging tool for comprehensive resistance profiling
3. Radiological Evaluation
- Chest X-ray may show bilateral infiltrates, cavitary lesions, or nodular opacities
- High-Resolution CT provides detailed imaging of bronchiectasis and fibrocavitary disease
Classification and Drug Resistance Profiles
Multidrug-Resistant TB (MDR-TB)
- Resistant to at least isoniazid and rifampin
Pre-Extensively Drug-Resistant TB (Pre-XDR-TB)
- MDR-TB plus resistance to any fluoroquinolone
Extensively Drug-Resistant TB (XDR-TB)
- MDR-TB with additional resistance to fluoroquinolones and at least one Group A drug (bedaquiline or linezolid)
Treatment of Pulmonary MDR-TB
The cornerstone of MDR-TB therapy involves a longer, more complex, and often more toxic regimen than that used for drug-susceptible TB. Treatment must be tailored based on drug sensitivity testing and guided by national or WHO recommendations.
1. Shorter Regimen (9–12 months)
- Used in selected patients without resistance to fluoroquinolones or second-line injectables.
- Includes bedaquiline, levofloxacin/moxifloxacin, clofazimine, ethambutol, pyrazinamide, and injectable agents like amikacin.
2. Longer Regimen (18–24 months)
- Indicated for cases with extensive resistance.
- Composed of at least four effective drugs:
- Bedaquiline
- Linezolid
- Clofazimine
- Cycloserine
- Delamanid or Pretomanid (based on availability)
3. New and Repurposed Drugs
- Bedaquiline: ATP synthase inhibitor, improves culture conversion rates
- Delamanid: Nitroimidazole with efficacy against MDR-TB
- Pretomanid: Used in combination regimens such as BPaL (Bedaquiline, Pretomanid, Linezolid)
4. Adverse Effects Management
- Frequent monitoring for QT prolongation, optic neuritis, hepatotoxicity, and myelosuppression
- Multidisciplinary management and pharmacovigilance required
Infection Control and Public Health Measures
Containing pulmonary MDR-TB requires strict adherence to airborne precautions and active case finding.
Key Measures
- Isolation of infectious patients
- Use of N95 respirators by healthcare workers
- Contact tracing and preventive therapy
- Community engagement and education
- Strengthened laboratory and surveillance systems
Prognosis and Outcomes
Pulmonary MDR-TB carries a lower treatment success rate (~60%) compared to drug-susceptible TB. Poor adherence, HIV coinfection, and extensive disease burden contribute to unfavorable outcomes. Early initiation of effective therapy significantly improves survival rates.
Future Directions in MDR-TB Management
- Universal access to rapid diagnostics
- Expanded use of all-oral regimens to reduce toxicity and improve adherence
- Host-directed therapies and immunomodulators under investigation
- Vaccination strategies beyond BCG, including subunit and mRNA-based candidates
Pulmonary multi-drug resistant Mycobacterium tuberculosis is a formidable threat to global TB control, necessitating robust diagnostic capabilities, personalized therapy, and coordinated public health strategies. Advancements in pharmacology, molecular diagnostics, and global health policy hold promise in mitigating the impact of MDR-TB and moving toward eventual eradication.