Pulmonary blastomycosis is a serious fungal infection that primarily affects the lungs. Caused by the Blastomyces dermatitidis fungus, this disease is commonly found in certain areas with high humidity, such as the Mississippi and Ohio River valleys, parts of the Great Lakes, and the southeastern United States. The infection can lead to severe respiratory issues if not diagnosed and treated early. While the disease is not highly contagious, it is a significant health concern for those living in endemic areas or individuals with compromised immune systems.
What is Pulmonary Blastomycosis?
Pulmonary blastomycosis is caused by the Blastomyces dermatitidis fungus, which is present in soil and decaying organic matter. The fungus thrives in moist environments and releases spores into the air that can be inhaled. Once inhaled, the spores can infect the lungs and cause symptoms that range from mild to severe. In severe cases, the infection can spread to other parts of the body, such as the skin, bones, and central nervous system, a condition known as disseminated blastomycosis.
Pathogenesis of Pulmonary Blastomycosis
The process begins when the spores of Blastomyces dermatitidis are inhaled into the respiratory tract. Once inside the lungs, the spores are converted into yeast-like cells that cause inflammation. This inflammation can lead to the formation of granulomas and abscesses, which may impair normal lung function. In rare cases, the infection can spread from the lungs to other organs, leading to more systemic manifestations.
Causes and Risk Factors
1. Exposure to Endemic Areas
The primary cause of pulmonary blastomycosis is exposure to the spores of Blastomyces dermatitidis. This fungus is endemic to specific regions, particularly in areas with high humidity and rich organic matter, such as:
- The Mississippi and Ohio River valleys
- The Great Lakes region
- Southeastern United States
People who live or work in these areas are at an increased risk of inhaling fungal spores, especially those who engage in outdoor activities such as hunting, camping, or construction.
2. Environmental Conditions Favoring Growth
Blastomyces thrives in moist, decaying organic matter, making areas with damp soil, wooded environments, or areas near rivers and lakes potential sources of infection. Occupational hazards are common among workers who disturb soil or other organic materials, such as farmers, miners, and construction workers.
3. Weakened Immune System
Individuals with compromised immune systems, such as those with HIV/AIDS, cancer patients undergoing chemotherapy, or individuals on long-term corticosteroid treatment, are more susceptible to developing pulmonary blastomycosis. In such individuals, the body’s ability to fight off fungal infections is diminished, leading to a higher risk of infection and more severe disease.
4. Male Gender and Age
Studies have shown that men, particularly those aged 30-50 years, are at a higher risk of developing pulmonary blastomycosis. This may be related to increased outdoor exposure and work-related activities that increase the likelihood of inhaling fungal spores.
Symptoms of Pulmonary Blastomycosis
The symptoms of pulmonary blastomycosis can vary greatly depending on the severity of the infection and the individual’s immune response. In some cases, the infection may be asymptomatic or cause only mild respiratory symptoms. In others, the infection can lead to more severe illness.
1. Respiratory Symptoms
The most common symptoms of pulmonary blastomycosis include:
- Cough: Often persistent and may produce sputum, sometimes tinged with blood.
- Shortness of Breath: Difficulty breathing, especially with physical exertion.
- Chest Pain: Pain that worsens with deep breathing or coughing.
- Wheezing: A high-pitched whistling sound during breathing.
2. Systemic Symptoms
In some cases, pulmonary blastomycosis can present with symptoms that affect the entire body, including:
- Fever: Common, particularly in more severe cases.
- Fatigue: Chronic tiredness that is not relieved by rest.
- Night Sweats: Profuse sweating during the night, often soaking bedclothes.
- Weight Loss: Unexplained weight loss due to systemic infection.
3. Complications in Severe Cases
If left untreated, pulmonary blastomycosis can progress to more severe complications, such as:
- Chronic pneumonia: Persistent lung infection that may lead to lung damage.
- Disseminated Blastomycosis: The infection can spread from the lungs to other organs, including the skin, bones, and nervous system, causing more widespread damage.
Diagnosing Pulmonary Blastomycosis
Accurate diagnosis of pulmonary blastomycosis involves several steps, including clinical evaluation, imaging studies, and laboratory tests.
1. Clinical Evaluation
The initial assessment involves a thorough medical history and physical examination. Key risk factors, such as exposure to endemic regions and pre-existing lung conditions, are considered. The clinician will also look for characteristic symptoms like persistent cough, chest pain, and fever.
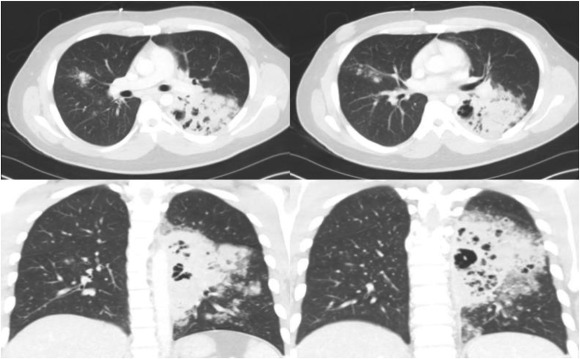
2. Imaging Studies
Chest X-rays or CT scans are crucial in evaluating lung damage caused by Blastomyces infection. In mild cases, the imaging may show diffuse lung infiltrates, while more severe cases may present with consolidation, cavities, or masses indicative of fungal growth.
3. Laboratory Tests
The diagnosis is confirmed through laboratory tests, including:
- Sputum Culture: A sample of sputum is cultured to detect the presence of Blastomyces.
- Urinary Antigen Test: A rapid test that can detect Blastomyces antigens in the urine, helping to diagnose blastomycosis.
- Serological Tests: Blood tests to detect antibodies or fungal antigens specific to Blastomyces can aid in diagnosis.
- Histopathological Examination: In severe cases, tissue samples from biopsies may be examined under a microscope for the characteristic yeast form of Blastomyces.
Treatment Options for Pulmonary Blastomycosis
The treatment of pulmonary blastomycosis depends on the severity of the infection and the patient’s overall health. Antifungal therapy is the mainstay of treatment, with options including:
1. Itraconazole
Itraconazole is the first-line treatment for non-disseminated pulmonary blastomycosis and is effective in controlling mild to moderate infections. It is taken orally and has fewer side effects compared to other antifungal agents.
2. Amphotericin B
For more severe cases, especially invasive pulmonary blastomycosis or disseminated infections, intravenous amphotericin B may be required. This powerful antifungal drug is effective but comes with potential side effects, such as kidney damage, and is typically administered in a hospital setting.
3. Fluconazole and Posaconazole
Fluconazole and posaconazole are used as alternatives or adjuncts to itraconazole in treating pulmonary blastomycosis, especially in patients who cannot tolerate itraconazole or have a resistant strain of the fungus.
4. Supportive Care
In addition to antifungal medications, supportive care is essential for managing symptoms and improving patient comfort. Oxygen therapy may be necessary for individuals with severe respiratory distress, and pain management for chest pain is crucial to enhance quality of life.
Preventing Pulmonary Blastomycosis
While it is difficult to completely prevent pulmonary blastomycosis, reducing exposure to Blastomyces spores can lower the risk of infection. Preventive measures include:
- Avoiding outdoor activities in areas known to have Blastomyces spores, especially during high-risk seasons.
- Wearing protective equipment like masks while working in environments that disturb soil or organic matter.
- Improving indoor air quality in areas prone to moisture and mold growth.
Prognosis of Pulmonary Blastomycosis
With prompt diagnosis and appropriate antifungal therapy, the prognosis for most patients with pulmonary blastomycosis is favorable, particularly for those with mild to moderate infections. However, untreated or severe cases may lead to chronic lung disease or systemic infection, which can significantly impact health.
Pulmonary blastomycosis is a potentially serious fungal infection that can affect the lungs and other organs if left untreated. Understanding the causes, symptoms, and treatment options is essential for managing this disease effectively. Early detection and the use of appropriate antifungal therapy can lead to successful outcomes and a return to normal lung function. By increasing awareness and taking preventive measures, individuals can reduce their risk of contracting this fungal infection.