Psychosis in Parkinson’s disease (PD) refers to the occurrence of hallucinations and delusions in patients diagnosed with Parkinson’s. This condition represents one of the most challenging non-motor symptoms associated with the disease, significantly impacting the patient’s quality of life and complicating their treatment regimen. Approximately 20% to 40% of individuals with Parkinson’s experience psychotic symptoms at some point during the progression of the disease.
Symptoms of Psychosis in Parkinson’s Disease
Psychosis in Parkinson’s disease is not a single symptom but a range of psychiatric disturbances that can greatly affect daily living. The most common symptoms include:
- Hallucinations: Most commonly visual, these involve seeing objects, people, or animals that aren’t present. Auditory hallucinations, though rarer, can also occur.
- Delusions: These are false beliefs that patients strongly hold despite evidence to the contrary. Common delusions in Parkinson’s psychosis include paranoid thoughts, such as believing that others are trying to harm them.
- Disorganized thinking: Patients may have trouble following conversations or connecting ideas in a coherent manner.
- Increased agitation or aggression: Emotional outbursts or frustration are often linked to the misinterpretation of surroundings or a distorted sense of reality.
- Depression and anxiety: These are often seen as co-existing symptoms due to the cognitive decline and frustration of dealing with the disease.
The Underlying Causes of Psychosis in Parkinson’s Disease
Psychosis in Parkinson’s disease is thought to arise from a combination of factors related to both the neurodegenerative nature of Parkinson’s and the medications used to treat it.
1. Neurodegeneration and Dopamine Imbalance
Parkinson’s disease is characterized by the progressive degeneration of dopamine-producing neurons in the brain, particularly in the substantia nigra. This depletion in dopamine levels is primarily responsible for the motor symptoms of Parkinson’s, such as tremors and rigidity. However, dopamine also plays a significant role in regulating mood and cognition. A disruption in dopamine pathways may contribute to the development of psychosis.
2. Medications for Parkinson’s Disease
The use of dopaminergic medications (such as levodopa) to manage motor symptoms can sometimes contribute to psychosis. These medications increase dopamine levels in the brain, which, while alleviating physical symptoms, can inadvertently provoke psychiatric disturbances, including hallucinations and delusions.
3. Disease Progression
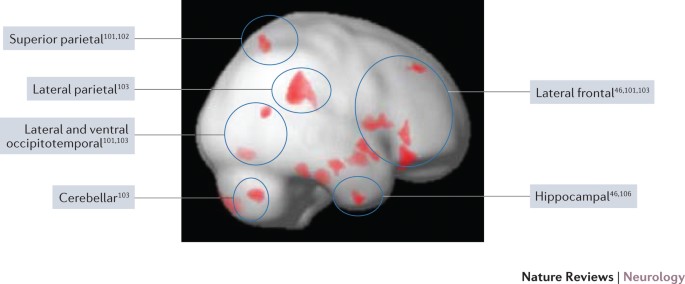
As Parkinson’s advances, the neurodegenerative process affects other brain regions, such as the frontal cortex and limbic system, areas involved in perception, emotional regulation, and reality testing. This progressive degeneration can increase the likelihood of developing psychotic symptoms.
4. Age and Cognitive Impairment
Older patients with Parkinson’s disease and those who experience cognitive decline or dementia are at a higher risk of developing psychosis. Cognitive impairment is often exacerbated by the presence of psychotic symptoms.
Diagnosing Psychosis in Parkinson’s Disease
Diagnosis of psychosis in Parkinson’s is primarily clinical, based on the presence of hallucinations or delusions in a patient with confirmed Parkinson’s disease. The diagnostic process involves:
- Patient history and psychiatric evaluation: A detailed history is essential, as psychotic symptoms can often be mistaken for other cognitive issues or medication-related side effects.
- Exclusion of other causes: It is important to rule out other potential causes of psychiatric disturbances, such as infections, metabolic imbalances, or other forms of dementia like Lewy body dementia.
- Neuroimaging and laboratory tests: These are used primarily to rule out other neurological conditions or complications.
Treatment of Psychosis in Parkinson’s Disease
Managing psychosis in Parkinson’s disease requires a balance between controlling the motor symptoms of Parkinson’s and minimizing the psychiatric disturbances. Treatment approaches include pharmacologic and non-pharmacologic strategies.
1. Non-Pharmacologic Interventions
Behavioral management and environmental changes are essential first-line approaches:
- Environmental modifications: A calm, well-lit environment can reduce the risk of hallucinations, particularly visual ones.
- Psychological support: Cognitive behavioral therapy (CBT) and caregiver support can help manage anxiety and paranoia.
- Routine management: Establishing a consistent daily routine can help reduce confusion and agitation.
2. Pharmacologic Treatments
In cases where non-pharmacologic approaches are insufficient, medications are considered:
- Atypical antipsychotics: Quetiapine and clozapine are often used to treat psychosis in Parkinson’s. These drugs are preferred because they have a lower risk of exacerbating motor symptoms, compared to older antipsychotics.
- Pimavanserin: This drug, a serotonin inverse agonist, is FDA-approved for treating Parkinson’s disease psychosis. It works by targeting serotonin receptors rather than dopamine, minimizing the risk of worsening motor symptoms.
- Clozapine: Used in more severe cases, though it requires careful monitoring due to its side effects, including agranulocytosis (a potentially life-threatening condition).
- Adjustments in dopaminergic medications: In some cases, lowering the dose or changing the timing of dopaminergic medications can reduce psychotic symptoms.
Long-Term Management and Prognosis
Psychosis associated with Parkinson’s disease is a chronic and progressive condition. The prognosis is variable, but with appropriate management, many patients can experience significant improvements in quality of life. Continuous monitoring is crucial, as the psychotic symptoms may evolve over time.
Patients may experience:
- A more rapid progression of Parkinson’s motor symptoms when psychosis is untreated.
- Increased risk of falls due to hallucinations or disorientation.
- Higher likelihood of institutionalization due to the complexity of managing both psychosis and Parkinson’s motor symptoms.
Frequently Asked Questions
What causes psychosis in Parkinson’s disease?
Psychosis in Parkinson’s can be caused by a combination of neurodegenerative processes, dopaminergic medication, and cognitive impairment.
Is psychosis common in Parkinson’s patients?
Yes, up to 40% of people with Parkinson’s experience psychosis at some point during their illness.
Can psychosis in Parkinson’s disease be treated?
Yes, psychosis can be treated using a combination of medications and behavioral interventions. Atypical antipsychotics and pimavanserin are common treatment options.
Are there any risks associated with treating Parkinson’s psychosis?
Some medications, especially dopaminergic agents, can worsen motor symptoms. Therefore, treatment must be carefully managed.
Psychosis in Parkinson’s disease is a complex and distressing aspect of the disease that requires tailored management strategies. By recognizing the symptoms early, understanding the underlying causes, and applying appropriate treatments, we can improve the outcomes for individuals living with Parkinson’s psychosis, offering them a better quality of life and supporting caregivers in their roles.

