Psychosis associated with Alzheimer’s disease (AD) represents a subset of neuropsychiatric symptoms characterized by delusions and hallucinations. These symptoms are not mere byproducts of memory loss but core clinical manifestations affecting 30% to 50% of individuals diagnosed with AD. Psychosis not only exacerbates cognitive decline but also accelerates functional deterioration, increases caregiver burden, and often results in institutionalization.
Clinical Presentation and Symptomatology
Psychotic symptoms in Alzheimer’s disease typically manifest during the middle to late stages and present distinct diagnostic and therapeutic challenges. The most common manifestations include:
- Delusions: Often paranoid in nature—beliefs that someone is stealing from them, their spouse is unfaithful, or people are plotting harm.
- Hallucinations: Primarily visual, involving the perception of people or animals that are not present.
- Disorganized thought: Reduced ability to logically connect ideas, often leading to confusion and agitation.
- Increased agitation or aggression: Frequently in response to misperceptions or delusional beliefs.
Unlike primary psychotic disorders such as schizophrenia, these symptoms occur in the context of progressive cognitive decline and are typically intermittent.
Etiology and Pathophysiology
The exact mechanisms leading to psychosis in Alzheimer’s remain under investigation, but current evidence suggests multifactorial origins:
- Neurodegeneration: Loss of cholinergic and serotonergic neurons in cortical and subcortical structures contributes to perceptual and cognitive disturbances.
- Amyloid and tau pathology: Greater deposition of tau protein in the frontal cortex correlates with psychotic symptoms.
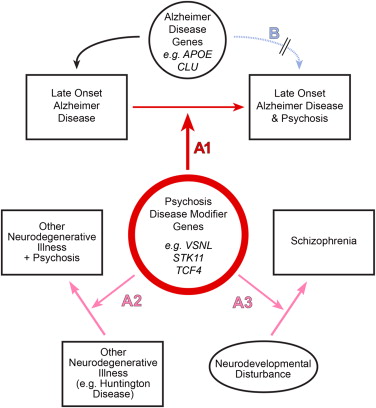
- Genetic predisposition: Polymorphisms in genes such as APOE-ε4 and those affecting dopamine signaling may influence risk.
- Environmental triggers: Changes in environment, caregiver interaction, or sensory deprivation can precipitate psychotic episodes.
Diagnostic Criteria for Alzheimer’s-Related Psychosis
Psychosis in AD is diagnosed clinically, guided by standardized criteria:
- Presence of delusions or hallucinations
- Duration of symptoms lasting ≥1 month
- Onset after AD diagnosis
- Exclusion of other medical or psychiatric conditions (e.g., delirium, schizophrenia)
- Confirmed cognitive impairment per DSM-5 or NIA-AA criteria
Neuroimaging and laboratory tests may be used to rule out other potential causes of behavioral change.
Differential Diagnosis
To ensure accurate treatment, differential diagnosis should exclude:
- Delirium: Acute onset, fluctuating course, usually reversible.
- Other dementias: Lewy body dementia often presents with earlier and more severe hallucinations.
- Medication side effects: Especially anticholinergics, opioids, or corticosteroids.
- Mood disorders: Depression with psychotic features can mimic some symptoms.
Management Strategies for Alzheimer’s-Related Psychosis
Treatment aims to reduce distress and improve quality of life, prioritizing safety and minimizing side effects.
Non-Pharmacologic Interventions
First-line management involves behavioral and environmental modifications:
- Consistent routine and familiar surroundings
- Redirection techniques and validation therapy
- Sensory stimulation and music therapy
- Caregiver education and support programs
Pharmacologic Treatments
When psychosis causes significant distress or danger, medications may be considered with caution:
- Atypical antipsychotics: Risperidone and aripiprazole show modest efficacy but carry risks of cerebrovascular events and mortality.
- Pimavanserin: A selective serotonin inverse agonist, FDA-approved for Parkinson’s disease psychosis, under investigation for AD psychosis.
- Cholinesterase inhibitors and memantine: May offer mild benefit on behavioral symptoms though primarily indicated for cognitive decline.
Prognosis and Outcomes
Psychosis in Alzheimer’s disease is linked to a poorer prognosis:
- Faster cognitive and functional decline
- Increased mortality rates
- Earlier institutionalization
- Higher caregiver stress and depression
Effective intervention, especially early behavioral approaches combined with careful pharmacologic use when necessary, can improve outcomes significantly.
Research and Future Directions
Emerging treatments and ongoing research focus on:
- Neuroinflammatory pathways: Targeting cytokines and microglial activation.
- Precision medicine: Genetic and biomarker profiling to tailor treatments.
- New pharmacologic agents: Such as serotonin receptor modulators and tau aggregation inhibitors.
- Digital behavioral therapy platforms: Enhancing access to non-pharmacologic interventions.
Frequently Asked Questions
How common is psychosis in Alzheimer’s disease?
Between 30% to 50% of individuals with Alzheimer’s experience psychosis during the disease course.
Can Alzheimer’s psychosis be cured?
No, but symptoms can be managed effectively through targeted therapies and supportive care.
Are hallucinations in Alzheimer’s always visual?
Mostly visual, but they can occasionally be auditory or tactile in advanced stages.
When should medication be used for Alzheimer’s-related psychosis?
Only when non-drug interventions fail and the patient or caregivers are at risk due to the symptoms.
What is the life expectancy after psychosis onset in Alzheimer’s?
Life expectancy varies, but psychosis typically indicates more rapid disease progression.
Psychosis in Alzheimer’s disease is a serious and often overlooked manifestation that significantly affects patient outcomes and caregiver burden. Through precise diagnosis, careful treatment planning, and ongoing research into innovative therapies, we can better manage this debilitating complication and enhance the lives of those affected by Alzheimer’s and their families.