Pseudomonas aeruginosa is the most common and persistent pathogen found in the respiratory tracts of individuals with cystic fibrosis (CF). Its ability to form biofilms, adapt to the mucus-rich environment of CF lungs, and develop multidrug resistance makes it a formidable challenge in long-term disease management. Chronic colonization often begins in adolescence and is associated with progressive pulmonary decline, increased morbidity, and reduced life expectancy.
Pathophysiology: How Pseudomonas Thrives in the CF Lung
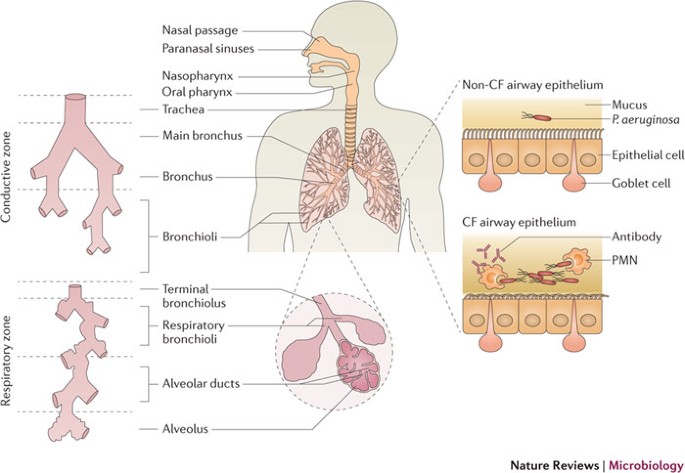
Cystic fibrosis, caused by mutations in the CFTR gene, results in thick, sticky mucus accumulation in the airways. This altered airway environment favors bacterial colonization and impairs mucociliary clearance.
Pathogenic Process of P. aeruginosa in CF Airways
Over time, the organism undergoes phenotypic changes—such as mucoid conversion—which further enhance persistence and immune resistance.
Epidemiology and Risk Factors for Chronic Colonization
- Prevalence: Approximately 60–80% of CF patients develop chronic P. aeruginosa colonization by adulthood.
- Risk Factors:
- Advanced age
- Repeated antibiotic exposure
- Environmental exposure (e.g., contaminated water sources)
- Previous respiratory infections or hospitalizations
- Genetic factors influencing mucus composition
Clinical Manifestations in Cystic Fibrosis Patients
The clinical impact of P. aeruginosa in CF varies depending on the infection stage:
Intermittent Colonization
- Transient detection in sputum cultures
- Often asymptomatic or associated with mild respiratory symptoms
Chronic Infection
- Persistent positive cultures over months
- Increased frequency of pulmonary exacerbations
- Daily cough with purulent sputum
- Progressive decline in FEV1 (Forced Expiratory Volume)
- Digital clubbing and failure to thrive in children
Diagnostic Tools for Detecting Pseudomonas in CF Airways
Sputum Culture and Molecular Techniques
- Routine sputum or oropharyngeal swab cultures in symptomatic and asymptomatic patients
- Quantitative PCR and 16S rRNA sequencing improve early detection
- Biofilm-related phenotypes, including mucoid strains, are particularly significant
Pulmonary Imaging
- High-resolution CT to detect bronchiectasis and mucus plugging
- Radiographic changes may precede culture positivity in early infection stages
Antibiotic Treatment Strategies
Effective management depends on the infection stage and susceptibility profile of the strain.
Eradication Therapy (First-Time Colonization)
- Inhaled tobramycin (28-day course)
- Oral ciprofloxacin ± inhaled colistin
- Nebulized levofloxacin or aztreonam in select cases
Chronic Suppressive Therapy
- Long-term inhaled antibiotics:
- Tobramycin inhalation solution (TIS)
- Aztreonam lysine for inhalation (AZLI)
- Colistimethate sodium
- Oral ciprofloxacin during exacerbations
- Intravenous ceftazidime, piperacillin-tazobactam, or meropenem for severe cases
Emerging Agents
- Ceftolozane-tazobactam and ceftazidime-avibactam for MDR strains
- Bacteriophage therapy (in development)
- Anti-biofilm peptides and quorum-sensing inhibitors
Pulmonary Exacerbations Linked to Pseudomonas Infection
Exacerbations are marked by:
- Increased cough and sputum production
- Decline in lung function (≥10% drop in FEV1)
- Malaise and weight loss
- Worsening radiographic findings
Prompt IV antibiotic therapy is critical to restoring baseline function and preventing irreversible damage.
Prevention and Long-Term Management
Airway Clearance and Maintenance
- Daily chest physiotherapy and mucolytics (e.g., dornase alfa)
- Hypertonic saline to improve mucus clearance
- Bronchodilators for airflow improvement
Infection Control
- Strict hygiene protocols in clinical settings
- Avoidance of cross-infection between CF patients
- Environmental precautions (e.g., avoidance of hot tubs, humidifiers)
Vaccination and Monitoring
- Annual influenza and pneumococcal vaccines
- Regular spirometry and sputum cultures
Role of Biofilms in Chronic Pseudomonas Infection
Biofilm formation is central to chronic colonization and antibiotic resistance. Within biofilms:
- Bacteria exhibit reduced metabolic activity, limiting antibiotic efficacy
- Polysaccharide matrix shields from host immune cells
- Horizontal gene transfer promotes resistance
Targeting biofilm pathways represents a future therapeutic direction.
Prognosis and Outcomes
Chronic P. aeruginosa infection is a critical determinant of CF prognosis:
- Accelerated pulmonary function decline
- Increased hospitalization and healthcare utilization
- Reduced quality of life and life expectancy
Early detection and aggressive eradication improve long-term outcomes significantly.
Frequently Asked Questions:
Q1. Why is Pseudomonas aeruginosa so common in CF lungs?
Thick, dehydrated mucus in CF lungs provides an ideal environment for colonization and biofilm formation.
Q2. Can Pseudomonas infection in CF be cured?
Initial infections may be eradicated; however, chronic colonization is often lifelong and managed rather than cured.
Q3. What is mucoid Pseudomonas and why is it important?
Mucoid strains overproduce alginate, promoting chronic infection and resistance to host defenses.
Q4. What role does inhaled antibiotic therapy play?
Inhaled antibiotics deliver high local concentrations directly to the lungs, improving efficacy and reducing systemic toxicity.
Q5. Is Pseudomonas infection the leading cause of death in CF?
While not the only cause, it significantly contributes to respiratory failure and mortality in cystic fibrosis patients.

