Pseudomonas aeruginosa pneumonia is a severe lower respiratory tract infection caused by a highly virulent gram-negative bacterium. Predominantly observed in healthcare settings, it is a major cause of hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP), particularly in immunocompromised or critically ill patients. Its intrinsic resistance mechanisms, ability to form biofilms, and adaptability make it one of the most challenging pathogens in pulmonary infections.
Epidemiology and High-Risk Populations
Pseudomonas aeruginosa ranks among the top three causes of nosocomial pneumonia worldwide. The following patient populations are especially vulnerable:
- Mechanically ventilated patients
- Individuals with cystic fibrosis or bronchiectasis
- Immunocompromised hosts (e.g., chemotherapy, transplant recipients)
- Patients with prolonged ICU stays
- Individuals with structural lung disease or previous broad-spectrum antibiotic use
Pathogenesis of Pseudomonas Lung Infection
Pseudomonas aeruginosa invades the pulmonary system through aspiration of contaminated secretions, inhalation of aerosols, or via hematogenous spread. Upon colonization, it utilizes several virulence factors including exotoxins, elastases, and quorum-sensing molecules that disrupt epithelial integrity and suppress immune responses.
Key Stages of Infection
Biofilm production further protects the bacteria from both immune defenses and antibiotics, contributing to chronicity and therapeutic resistance.
Clinical Features and Radiological Findings
Pseudomonas pneumonia may present acutely or insidiously, with symptoms varying in severity depending on host immunity and underlying conditions.
Common Clinical Manifestations
- High-grade fever
- Productive cough with green or purulent sputum
- Pleuritic chest pain
- Shortness of breath and hypoxia
- Rales or bronchial breath sounds on auscultation
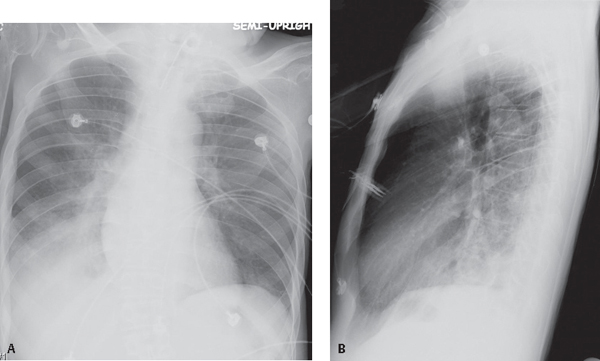
Radiographic Characteristics
- Unilateral or bilateral infiltrates, often in lower lobes
- Cavitary lesions or necrotizing pneumonia
- Air bronchograms in consolidation zones
- CT scans reveal abscess formation and bronchiectasis in chronic cases
Diagnostic Approach to Pseudomonas Pneumonia
Microbiological Confirmation
Definitive diagnosis requires isolating P. aeruginosa from respiratory specimens:
- Sputum Gram stain and culture
- Endotracheal aspirate or bronchoalveolar lavage (BAL) in intubated patients
- Blood cultures in severe or systemic infections
Biomarkers and Supportive Tests
- Elevated CRP and procalcitonin may indicate bacterial infection
- Leukocytosis with left shift
- Pulse oximetry and ABG to assess respiratory compromise
Antimicrobial Therapy and Resistance Patterns
Timely and effective antibiotic therapy is essential, especially in multidrug-resistant (MDR) or extensively drug-resistant (XDR) strains.
Empirical Therapy for High-Risk Patients
Initiate broad-spectrum coverage targeting Pseudomonas in the following combinations:
- Antipseudomonal beta-lactam (e.g., piperacillin-tazobactam, cefepime, ceftazidime)
- Plus fluoroquinolone (ciprofloxacin or levofloxacin) or aminoglycoside
- Consider carbapenems (e.g., meropenem) in resistant settings
Targeted Therapy Based on Culture Sensitivity
Adjust regimen once susceptibility results are available:
- Monotherapy for susceptible strains may include ceftazidime or cefepime
- Combination therapy is preferred for resistant or severe infections
- Duration: typically 7–14 days, extended if complications arise
Emerging Resistance Mechanisms
- Efflux pump activation
- Beta-lactamase and carbapenemase production
- Mutations in porin channels
- Horizontal gene transfer via plasmids
These mechanisms often result in treatment failures and prolonged ICU stays.
Adjunctive Treatments and Supportive Care
- Oxygen supplementation or mechanical ventilation
- Chest physiotherapy to assist in mucus clearance
- Bronchodilators in obstructive pulmonary disease
- Monitoring of renal function due to nephrotoxic potential of aminoglycosides
- Nutritional support and tight glycemic control in ICU patients
Complications and Prognosis
Complications of P. aeruginosa pneumonia can be life-threatening, including:
- Acute respiratory distress syndrome (ARDS)
- Sepsis and multi-organ dysfunction
- Pulmonary abscesses or empyema
- Chronic lung colonization and fibrosis in survivors
Mortality rates for Pseudomonas pneumonia range from 30–50%, particularly in MDR cases or delayed treatment scenarios.
Prevention and Infection Control
Preventive strategies are critical in healthcare environments:
- Strict hand hygiene and barrier precautions
- Surveillance cultures and isolation of colonized patients
- Minimizing duration of mechanical ventilation
- Selective digestive decontamination in high-risk ICUs
- Antimicrobial stewardship to reduce selective pressure
Frequently Asked Questions
Q1. What is the primary cause of Pseudomonas aeruginosa pneumonia?
It commonly arises from aspiration in ventilated patients or from colonization in immunocompromised individuals.
Q2. Is Pseudomonas pneumonia contagious?
While not highly contagious, it can spread in hospital settings through contaminated equipment or poor hygiene.
Q3. Can Pseudomonas pneumonia be cured?
Yes, with prompt diagnosis and appropriate antibiotic therapy, most cases can be treated successfully, although resistant infections pose challenges.
Q4. How long does treatment usually last?
Typically 7–14 days, but treatment may be extended in the presence of complications or MDR organisms.
Q5. What makes this pneumonia more dangerous than others?
Its ability to resist antibiotics and form protective biofilms often leads to severe infections and higher mortality.