Pseudomonas aeruginosa meningitis represents a severe and potentially fatal central nervous system (CNS) infection, predominantly observed in hospital settings, especially following neurosurgical procedures or head trauma. As a multidrug-resistant, gram-negative bacillus, P. aeruginosa poses considerable diagnostic and therapeutic challenges. This guide presents a complete overview of the pathogenesis, clinical features, diagnostic modalities, and current treatment options for this high-risk infection.
Pathogenesis of Pseudomonas Aeruginosa CNS Infection
Pseudomonas aeruginosa can breach the CNS via several pathways, particularly in immunocompromised individuals and neurosurgical patients. Once inside the subarachnoid space, it induces intense inflammation, leading to increased intracranial pressure and neuronal damage.
Routes of CNS Invasion
- Post-neurosurgical colonization (ventriculoperitoneal shunts, craniotomy)
- Skull fractures with CSF leaks
- Hematogenous dissemination from distant infection sites
- Direct inoculation during trauma or invasive procedures
Clinical Presentation of Pseudomonas Meningitis
The symptoms of P. aeruginosa meningitis are often severe and progress rapidly. Early recognition is vital for reducing morbidity and mortality.
Key Signs and Symptoms
- High-grade fever
- Altered mental status
- Neck stiffness
- Photophobia
- Nausea and vomiting
- Seizures
- Focal neurologic deficits (in advanced cases)
- Signs of increased intracranial pressure (e.g., papilledema)
In post-neurosurgical patients, fever and changes in consciousness are often the only early indicators.
Risk Factors for Pseudomonas Aeruginosa Meningitis
The following conditions predispose individuals to P. aeruginosa CNS infections:
- Neurosurgical procedures (e.g., external ventricular drains, shunts)
- Penetrating cranial trauma
- Hospital-acquired bacteremia
- Immunosuppression (e.g., neutropenia, transplant recipients)
- CSF leaks
- Extended ICU stays and prolonged intubation
- Previous antibiotic use altering normal flora
Diagnostic Evaluation: Identifying Pseudomonal CNS Infection
Timely diagnosis of P. aeruginosa meningitis is crucial and typically requires a combination of laboratory and imaging studies.
Cerebrospinal Fluid (CSF) Analysis
- Appearance: Turbid or purulent
- Elevated WBC count (neutrophilic predominance)
- Low glucose concentration
- Elevated protein levels
- Gram stain: Gram-negative rods
- CSF culture: Definitive identification of P. aeruginosa
- PCR testing: Rapid identification and resistance gene profiling
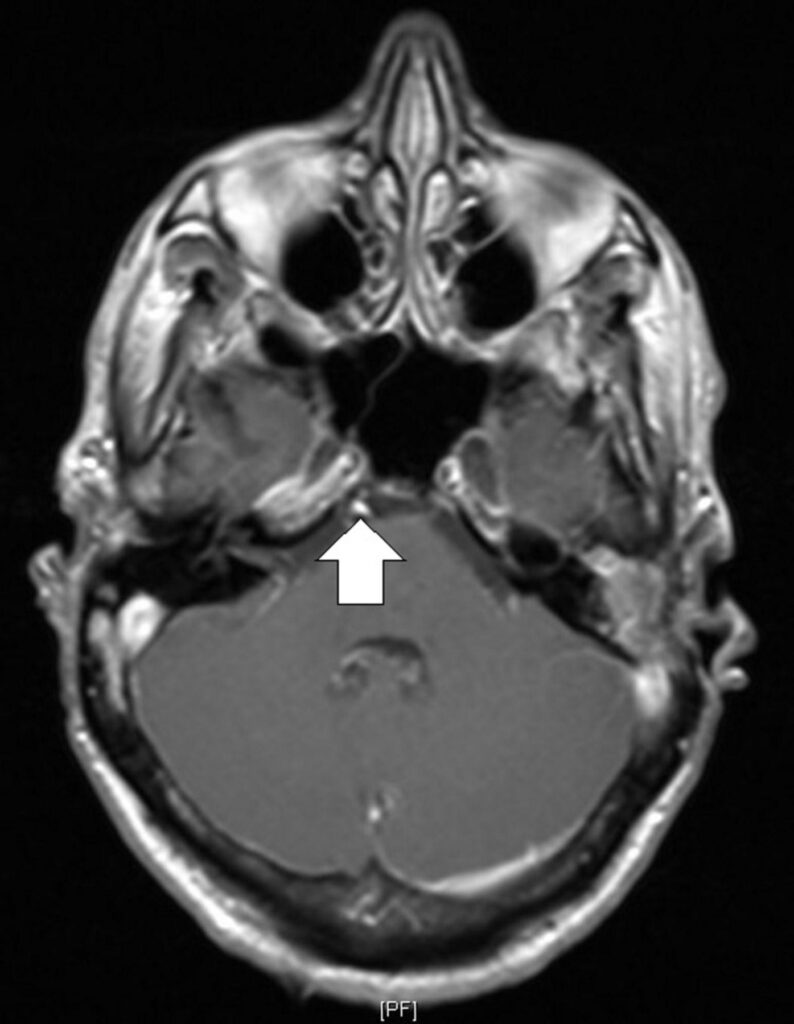
Imaging Studies
- CT/MRI brain: Rule out hydrocephalus, abscess, ventriculitis, or cerebral edema
Antibiotic Treatment Protocols for Pseudomonas Meningitis
Effective therapy hinges on early empirical treatment tailored to known or suspected antibiotic susceptibility.
Empirical Coverage
- Cefepime or Meropenem: Broad-spectrum anti-pseudomonal activity
- Combination with Aminoglycosides (e.g., amikacin): In synergistic cases
- Consider Ceftazidime or Ceftolozane-tazobactam for MDR strains
Intrathecal or Intraventricular Therapy
In cases with poor response to intravenous antibiotics or the presence of CSF devices:
- Colistin or Tobramycin may be administered intraventricularly under strict monitoring.
Treatment Duration
- Minimum 14–21 days of parenteral antibiotics
- Extended therapy required for device-associated infections or abscess formation
Neurosurgical Interventions and Device Management
When meningitis is associated with foreign bodies (e.g., shunts, drains), surgical management is often necessary.
- Removal or replacement of infected hardware
- Ventricular irrigation in selected cases
- Drainage of abscesses or empyemas if identified radiologically
Prognosis and Outcomes
Despite aggressive treatment, the prognosis of P. aeruginosa meningitis remains guarded, especially in patients with multidrug-resistant strains or delayed intervention.
Prognostic Indicators
- Time to appropriate antibiotic initiation
- Severity of neurologic symptoms on presentation
- Presence of hydrocephalus or cerebral edema
- Success of source control (e.g., device removal)
- Patient’s baseline immune status
Mortality rates range from 30–50%, and survivors may experience lasting neurologic sequelae, including cognitive deficits, hearing loss, or seizures.
Prevention Strategies in Healthcare Settings
Preventing pseudomonal meningitis requires rigorous adherence to infection control practices, especially in neurosurgical environments.
- Sterile technique during CNS procedures
- Antimicrobial prophylaxis in high-risk surgeries
- Strict device care protocols for EVDs and shunts
- Surveillance cultures in ICU and neurosurgery wards
- Antibiotic stewardship to prevent resistance development
Pseudomonas aeruginosa meningitis represents a formidable clinical entity that demands immediate recognition, accurate microbiological diagnosis, and tailored antimicrobial therapy. Given its predilection for neurosurgical patients and the critically ill, a multidisciplinary approach encompassing infectious disease, neurology, and surgery is imperative to improving outcomes and reducing long-term complications.