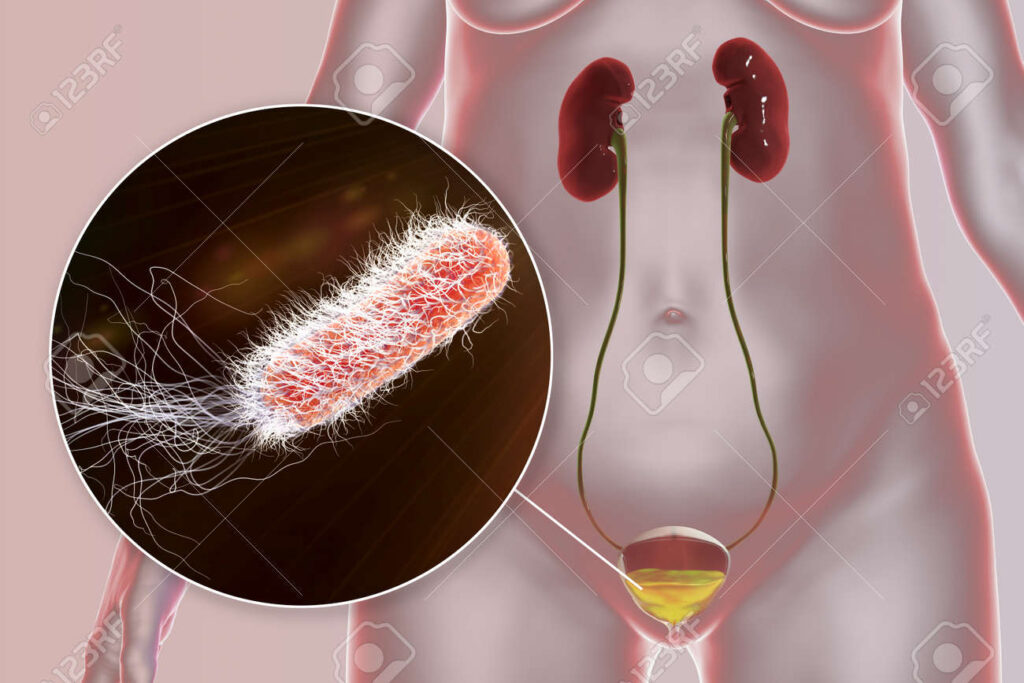
Pseudomonas aeruginosa cystitis is a complex form of urinary tract infection (UTI) often encountered in healthcare-associated settings and patients with underlying urological conditions. Known for its intrinsic resistance and biofilm-forming ability, this opportunistic pathogen presents significant therapeutic challenges, particularly in immunocompromised individuals and those with recurrent UTIs.
Overview of Pseudomonas Aeruginosa as a Uropathogen
P. aeruginosa is a gram-negative, aerobic bacillus with robust environmental adaptability and resistance mechanisms. Unlike common uropathogens like Escherichia coli, P. aeruginosa frequently colonizes patients with long-term catheterization, structural urinary tract anomalies, or prior antibiotic exposure.
Key Characteristics
- Non-fermenting, oxidase-positive
- Flagella-driven motility
- Produces pigments like pyocyanin
- Forms biofilms on urological devices
Epidemiology and Risk Factors for Pseudomonas Cystitis
Healthcare-associated infections (HAIs) and complex urologic cases account for the majority of P. aeruginosa cystitis cases. The risk is markedly elevated in:
- Indwelling urinary catheter users
- Recent urologic procedures or instrumentation
- Chronic urinary retention
- Neurogenic bladder dysfunction
- Hospitalization with broad-spectrum antibiotic use
Nosocomial prevalence is notably higher in intensive care and long-term care units, where antimicrobial resistance rates are also elevated.
Clinical Manifestations of Pseudomonas Cystitis
The symptomatology of P. aeruginosa cystitis often mimics other bacterial UTIs but tends to be more persistent and refractory to initial therapy. Common presentations include:
- Dysuria (painful urination)
- Urgency and frequency
- Suprapubic discomfort
- Hematuria (blood in urine)
- Foul-smelling, cloudy urine
- Fever and chills in upper tract involvement
Persistent or recurrent symptoms despite antibiotic therapy should prompt suspicion of Pseudomonas infection.
Pathophysiology and Infection Pathways
P. aeruginosa typically accesses the bladder through the ascending route, especially in catheterized individuals or those with vesicoureteral reflux. It adheres to uroepithelial surfaces, forms biofilms, and evades host immune responses.
Biofilm presence is particularly problematic, contributing to recurrent infections and antibiotic resistance.
Diagnostic Evaluation for Pseudomonas Aeruginosa Cystitis
Urine Culture and Sensitivity
The cornerstone of diagnosis involves quantitative urine culture, ideally collected through midstream clean-catch or catheterized specimen. P. aeruginosa typically exhibits:
- Growth on MacConkey agar as non-lactose fermenting colonies
- Characteristic greenish pigment and grape-like odor
- Resistance to common UTI antibiotics (e.g., TMP-SMX, nitrofurantoin)
Additional Tests
- Urinalysis: Pyuria and bacteriuria
- Imaging (if recurrent): Ultrasound or CT urogram to evaluate for structural abnormalities or stones
- Cystoscopy: In chronic or complicated cases to assess mucosal integrity
Antimicrobial Resistance and Therapeutic Approach
Resistance Profile
P. aeruginosa demonstrates resistance via:
- Efflux pumps
- Beta-lactamases (including AmpC and ESBLs)
- Reduced outer membrane permeability
- Biofilm-mediated tolerance
Multidrug-resistant (MDR) strains are increasingly common, particularly in nosocomial settings.
Recommended Antibiotic Regimens
Empiric therapy should be guided by local antibiograms and tailored upon sensitivity results. Effective agents include:
- Ciprofloxacin (if susceptible)
- Cefepime
- Piperacillin-tazobactam
- Carbapenems (e.g., meropenem)
- Aminoglycosides (e.g., gentamicin)
For MDR or XDR strains, colistin or ceftolozane-tazobactam may be required.
Non-Antibiotic Management and Adjunctive Strategies
- Catheter removal or replacement is imperative in catheter-associated infections.
- Increased fluid intake to flush the urinary tract.
- Bladder irrigation in select cases under urological guidance.
- Surgical correction for structural anomalies contributing to infection persistence.
Probiotics and cranberry extract have limited efficacy in Pseudomonas infections due to its unique pathogenic traits.
Prevention of Pseudomonas Aeruginosa Cystitis
Preventive measures focus on minimizing modifiable risk factors:
- Strict catheter protocols: Use only when necessary, aseptic insertion, and timely removal.
- Antibiotic stewardship to limit resistance development.
- Hydration promotion in at-risk individuals.
- Hygienic practices in hospitals and care facilities.
Prognosis and Long-Term Management
The prognosis of P. aeruginosa cystitis largely depends on early recognition and appropriate antimicrobial therapy. However, recurrence is common without correcting underlying risk factors. Chronic colonization and relapsing infections require coordinated care between urologists and infectious disease specialists.
Pseudomonas aeruginosa cystitis represents a challenging clinical entity, particularly in vulnerable or hospitalized populations. Its resistance profile, combined with biofilm-associated persistence, mandates precision in diagnosis and aggressiveness in therapy. With vigilant preventive strategies and evidence-based management, we can reduce the burden and recurrence of this difficult-to-treat infection.