Complicated appendicitis—marked by perforation, abscess formation, or gangrene—poses a heightened risk for infection with multidrug-resistant organisms such as Pseudomonas aeruginosa. Recognized for its adaptability and intrinsic resistance mechanisms, this gram-negative bacterium significantly influences therapeutic strategies, recovery time, and prognosis.
Pathogenesis of Pseudomonas Aeruginosa in Appendiceal Infections
P. aeruginosa is not a primary colonizer of the normal gastrointestinal flora but frequently emerges in hospitalized patients or those exposed to broad-spectrum antibiotics. In complicated appendicitis, the bacterial infiltration often occurs post-perforation, when mucosal barriers are compromised.
This transition from a sterile environment to an infection-prone site allows opportunistic pathogens like P. aeruginosa to proliferate, especially in nosocomial environments.
Risk Factors for Pseudomonas-Associated Appendicitis
Patients who develop P. aeruginosa infections in the context of appendicitis often share common clinical characteristics:
- Previous hospitalization or surgery
- Immunocompromised states (e.g., diabetes, cancer)
- Use of broad-spectrum antibiotics prior to admission
- Prolonged duration of symptoms before surgical intervention
- Intra-abdominal contamination or peritonitis
Such conditions disrupt the intestinal microbiota, reducing colonization resistance and facilitating Pseudomonas translocation.
Clinical Presentation of Pseudomonas-Complicated Appendicitis
While the signs of complicated appendicitis are consistent across causative organisms, P. aeruginosa infections often lead to more aggressive and persistent symptoms:
- High-grade fever and systemic signs of sepsis
- Diffuse abdominal pain, often shifting to the right lower quadrant
- Rebound tenderness and guarding
- Purulent discharge or abscess on imaging
- Postoperative wound infection or delayed healing
Persistent fever and leukocytosis after appendectomy may also suggest P. aeruginosa involvement.
Diagnostic Strategies: Confirming Pseudomonas in Appendiceal Complications
Microbiological Confirmation
Definitive diagnosis involves isolation of P. aeruginosa from:
- Peritoneal fluid cultures
- Surgical wound cultures
- Postoperative intra-abdominal abscesses
Culture results guide targeted antibiotic therapy and influence clinical outcomes.
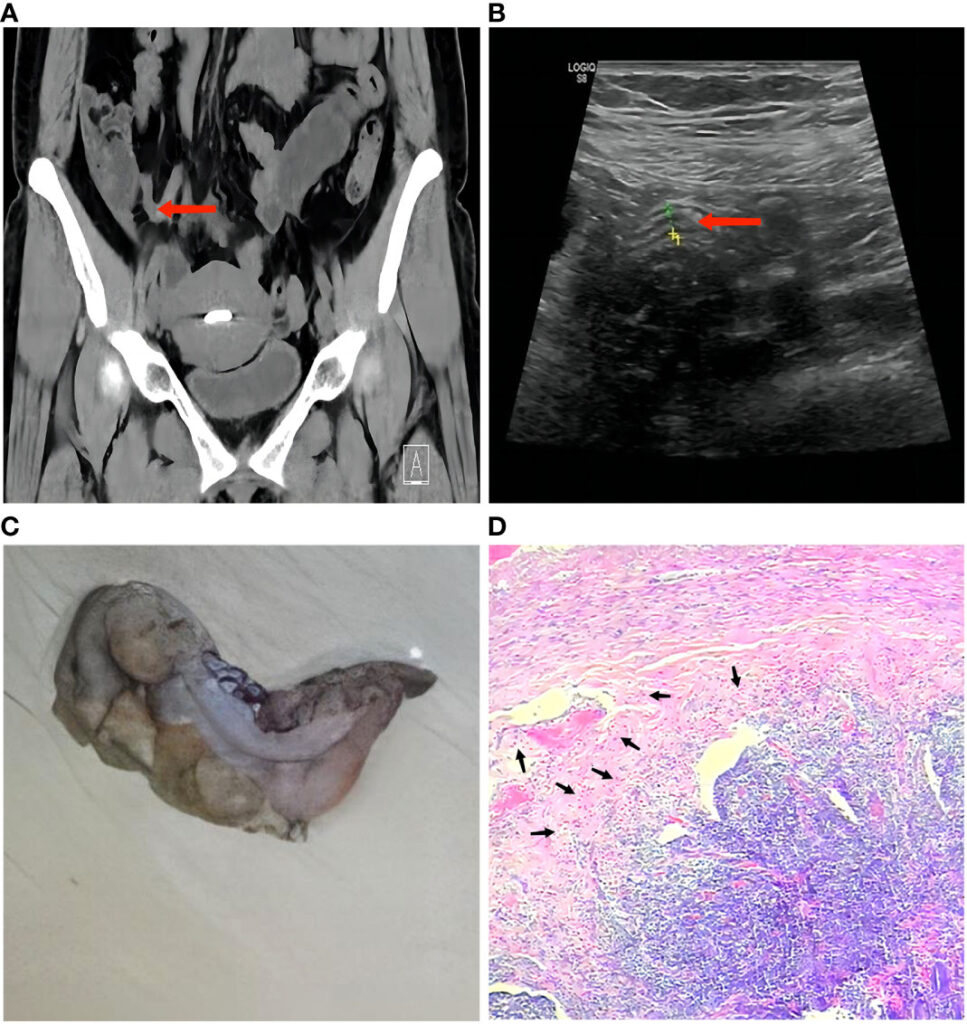
Imaging Support
- CT Abdomen: Crucial for detecting abscesses, perforation, and signs of peritonitis.
- Ultrasound: May reveal fluid collections or inflamed appendix, especially in children.
Antimicrobial Resistance and Therapeutic Implications
P. aeruginosa in intra-abdominal infections presents a formidable treatment challenge due to its resistance to many commonly used antibiotics.
Common Resistance Mechanisms
- Efflux pumps and porin mutations
- Extended-spectrum beta-lactamase (ESBL) production
- Biofilm formation within abscess cavities
Optimal Treatment Protocols for Pseudomonas-Associated Appendicitis
Empiric and Definitive Antibiotic Therapy
Initial empiric coverage for patients at risk should include antipseudomonal agents. Upon confirmation, therapy should be refined:
- Piperacillin-tazobactam
- Cefepime
- Carbapenems (meropenem or imipenem) for MDR strains
- Aminoglycosides or colistin in refractory cases
Duration of therapy typically spans 7–14 days, depending on clinical response and resolution of abscess or peritonitis.
Surgical Considerations
- Prompt laparoscopic or open appendectomy
- Drainage of abscesses either surgically or percutaneously
- Irrigation and debridement for wound infections
Early surgical intervention mitigates systemic spread and optimizes outcomes.
Postoperative Management and Follow-Up
Patients with Pseudomonas-associated complicated appendicitis require rigorous postoperative surveillance:
- Serial imaging for abscess resolution
- Monitoring for antibiotic-associated complications
- Assessment of nutritional and immune status in prolonged recovery
Regular follow-up is essential to detect recurrent infections, particularly in immunocompromised individuals.
Prevention and Risk Mitigation in Surgical Settings
Preventing P. aeruginosa involvement in appendicitis involves a multi-pronged infection control approach:
- Antibiotic stewardship to reduce resistance development
- Strict aseptic techniques in the operating room
- Early surgical intervention to prevent perforation
- Surveillance cultures in high-risk wards (e.g., ICU)
Education of healthcare professionals on recognizing early signs of complicated infections is vital.
Pseudomonas aeruginosa complicated appendicitis presents a distinct clinical challenge due to its aggressive nature, resistance profile, and associated morbidity. Early identification, combined with precise antimicrobial therapy and surgical intervention, remains the cornerstone of effective management. Preventive strategies and postoperative vigilance are crucial in reducing recurrence and improving patient outcomes in the context of this serious intra-abdominal infection.