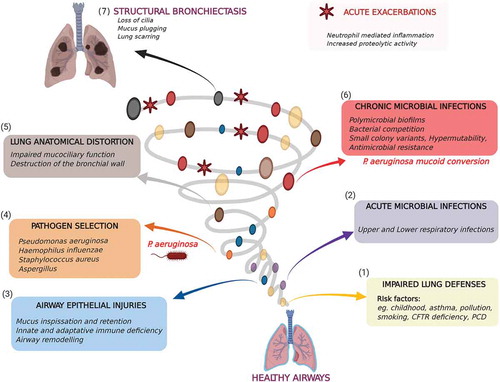
Pseudomonas aeruginosa bronchitis represents a serious respiratory tract infection primarily affecting individuals with underlying pulmonary diseases, immunosuppression, or structural lung abnormalities. This opportunistic pathogen poses significant clinical challenges due to its high antibiotic resistance and ability to form biofilms in the respiratory mucosa.
Pathophysiology of Pseudomonas Aeruginosa in Bronchial Infections
P. aeruginosa is a gram-negative, rod-shaped bacterium known for its adaptability and survival in hostile environments, including the human bronchial tree. Its presence in the lower airways is often associated with:
- Biofilm formation, especially on damaged epithelium
- Production of virulence factors (e.g., elastase, exotoxins)
- Induction of neutrophilic inflammation
- Chronic colonization in patients with bronchiectasis or COPD
Risk Factors Contributing to Pseudomonas Bronchitis
The development of Pseudomonas aeruginosa bronchitis is rarely spontaneous and typically follows a predisposing condition or prolonged hospital exposure.
Common Risk Factors
- Chronic obstructive pulmonary disease (COPD)
- Bronchiectasis
- Cystic fibrosis (CF)
- Prolonged mechanical ventilation
- Immunosuppressive therapy
- Previous antibiotic use altering normal flora
Clinical Manifestations: Symptoms of Pseudomonas Bronchitis
While symptoms may vary depending on the patient’s comorbidities and the acuteness of infection, common presentations include:
- Persistent productive cough with green or yellow sputum
- Shortness of breath and wheezing
- Fever and malaise (in acute exacerbations)
- Chest discomfort
- Signs of systemic inflammation (elevated CRP, leukocytosis)
Chronic colonization may occur without acute symptoms but contributes to long-term lung function decline.
Diagnostic Evaluation and Microbiological Confirmation
Clinical Workup
Diagnosis requires correlation between clinical features and laboratory evidence of infection:
- Sputum Gram stain and culture: Confirmation of P. aeruginosa presence
- Pulmonary function tests: Especially relevant in patients with underlying chronic lung disease
- Chest imaging (X-ray or CT scan): To identify structural lung changes
Microbiological Considerations
- Biofilm-associated strains often exhibit multi-drug resistance
- Repeated cultures may be required in chronic colonization to distinguish infection from colonization
Antimicrobial Resistance Patterns and Treatment Challenges
P. aeruginosa exhibits multiple resistance mechanisms, including:
- Efflux pump activation
- Beta-lactamase production (including ESBL and carbapenemase)
- Mutations in porins limiting drug entry
These factors necessitate tailored antibiotic strategies based on sensitivity testing.
Evidence-Based Treatment of Pseudomonas Aeruginosa Bronchitis
Empiric and Targeted Therapy
Initial empiric therapy should be adjusted based on culture and sensitivity data. Commonly used antibiotics include:
- Piperacillin-tazobactam
- Cefepime or ceftazidime
- Meropenem (especially in resistant strains)
- Aminoglycosides (e.g., tobramycin) as adjunct therapy
- Inhaled antibiotics (e.g., colistin or tobramycin) for chronic cases
Treatment duration: Typically ranges from 7 to 14 days, longer for chronic or relapsing cases.
Adjunctive Therapies and Supportive Management
Treatment success often requires more than antibiotics.
Supportive Measures
- Airway clearance techniques (physiotherapy, mucolytics)
- Bronchodilators to ease breathing
- Anti-inflammatory agents (e.g., macrolides in certain chronic cases)
- Smoking cessation for COPD patients
Prevention Strategies in High-Risk Populations
Preventing P. aeruginosa bronchitis requires targeted strategies in vulnerable individuals.
Key Preventive Measures
- Avoidance of unnecessary antibiotics
- Proper care and sterilization of respiratory devices
- Vaccination against respiratory pathogens
- Regular monitoring in bronchiectasis or CF patients
- Prompt management of exacerbations
Prognosis and Long-Term Outcomes
The prognosis of P. aeruginosa bronchitis depends on underlying health, timeliness of intervention, and effectiveness of infection control. Chronic colonization in structural lung diseases is associated with:
- Accelerated decline in lung function
- Increased frequency of exacerbations
- Higher hospitalization rates
Early identification and targeted therapy significantly improve outcomes.
Pseudomonas aeruginosa bronchitis is a complex and often recurrent infection that thrives in vulnerable respiratory environments. Optimal outcomes hinge on a high index of suspicion, robust diagnostic evaluation, and a strategic combination of antimicrobial and supportive therapies. Vigilant prevention, especially in patients with chronic pulmonary diseases, is vital to minimizing its burden and improving respiratory health.