Pseudomonas aeruginosa biliary tract infection represents a severe and potentially life-threatening condition involving the invasion of the biliary system by the opportunistic gram-negative bacterium P. aeruginosa. These infections, often hospital-acquired, require prompt diagnosis and targeted antimicrobial therapy due to the pathogen’s intrinsic resistance mechanisms and the vulnerability of the affected patients.
Understanding the Pathogen: Pseudomonas aeruginosa in the Biliary System
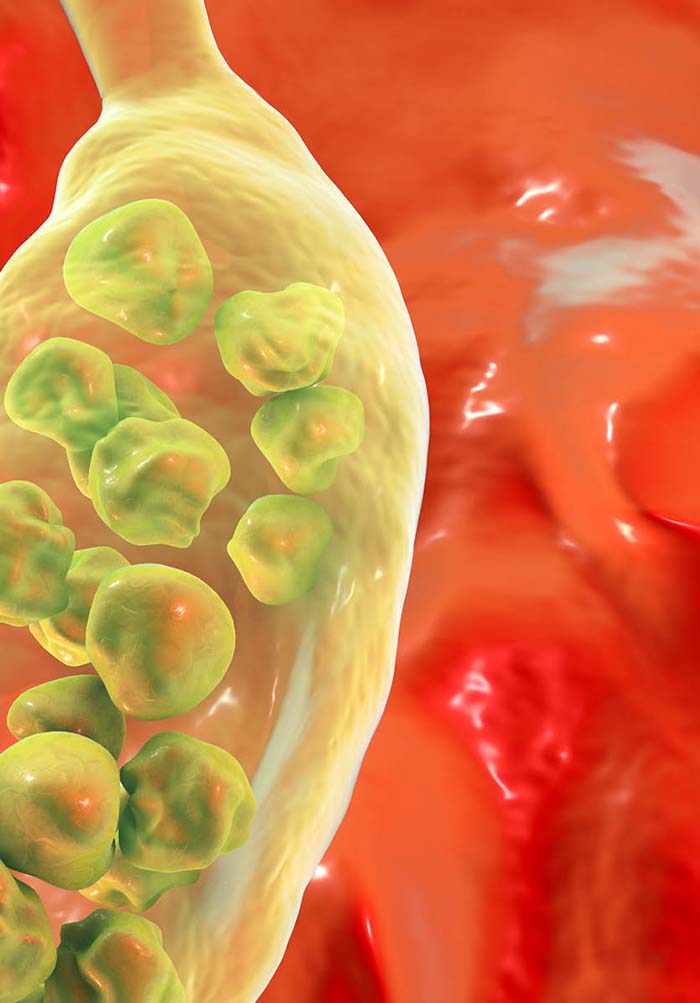
Pseudomonas aeruginosa is a motile, aerobic, gram-negative bacillus renowned for its resistance to many antibiotics. It typically affects immunocompromised hosts, patients with biliary stents, or those who have undergone surgical or endoscopic interventions in the hepatobiliary system.
Key Features of P. aeruginosa:
- Exhibits biofilm formation on biliary devices
- Produces exotoxins that impair host defenses
- Often found in nosocomial infections including biliary sepsis
Causes and Risk Factors for Pseudomonas Biliary Tract Infection
The biliary tract becomes susceptible to P. aeruginosa colonization and infection under specific predisposing conditions.
Predisposing Factors
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Biliary stenting or drainage devices
- Previous antibiotic therapy altering normal flora
- Immunosuppression (e.g., post-transplant, chemotherapy)
- Structural abnormalities such as biliary strictures or cholangitis
Clinical Presentation: Recognizing the Symptoms of Infection
Patients typically present with signs and symptoms consistent with acute cholangitis or biliary sepsis.
Common Clinical Features
- Fever and chills
- Right upper quadrant abdominal pain
- Jaundice
- Nausea and vomiting
- Hypotension and confusion in septic cases
The classic Charcot’s triad (fever, RUQ pain, jaundice) and Reynolds’ pentad (adding hypotension and altered mental status) are often seen in severe cases.
Diagnostic Approach to Pseudomonas Aeruginosa Biliary Infection
Laboratory Investigations
- Complete blood count: Elevated WBC count
- Liver function tests: Elevated alkaline phosphatase, GGT, bilirubin
- Blood cultures: Identification of P. aeruginosa in septicemia
- Bile cultures: Direct evidence from ERCP-guided sampling
Imaging Techniques
- Ultrasound: Detects biliary dilation and stones
- CT Scan or MRI/MRCP: Provides detailed visualization of biliary anatomy and complications
Antibiotic Resistance and Challenges in Treatment
P. aeruginosa displays intrinsic and acquired resistance mechanisms, complicating treatment.
Mechanisms of Resistance
- Efflux pumps and reduced permeability
- Beta-lactamase production (including ESBLs and carbapenemases)
- Biofilm formation on biliary prostheses
Effective Antimicrobial Therapy for Pseudomonas Biliary Infection
Timely administration of appropriate antibiotics is critical.
Empiric Therapy (Adjusted Upon Culture Results)
- Piperacillin-tazobactam
- Cefepime
- Meropenem (for suspected ESBL-producing strains)
- Aminoglycosides or fluoroquinolones in combination therapies
Duration: Typically 10–14 days, depending on clinical response and source control.
Interventional Management and Source Control
Infections associated with obstruction or indwelling devices often require procedural intervention.
Recommended Interventions
- Biliary drainage: Via ERCP or percutaneous transhepatic approach
- Removal or exchange of infected biliary stents
- Surgical drainage in complicated or refractory cases
Prognosis and Complications of Untreated or Delayed Management
Untreated infections can rapidly progress to biliary sepsis, multi-organ dysfunction, and death.
Potential Complications
- Liver abscess formation
- Persistent biliary strictures
- Secondary bloodstream infections
- Septic shock
Early recognition, microbiological diagnosis, and combined medical-surgical therapy are essential for favorable outcomes.
Preventive Strategies in High-Risk Patients
Preventive measures play a crucial role in minimizing recurrence and nosocomial transmission.
Best Practices
- Strict aseptic technique during ERCP and biliary procedures
- Minimizing duration of indwelling stents
- Targeted antibiotic prophylaxis in immunocompromised patients
- Regular monitoring of stent function and biliary patency
Pseudomonas aeruginosa biliary tract infections demand high clinical suspicion, especially in patients with prior biliary interventions or immunosuppression. With the growing challenge of antimicrobial resistance, a multidisciplinary approach combining timely diagnostics, precision antimicrobial therapy, and effective source control remains the cornerstone of management. Recognizing the early signs and instituting appropriate intervention significantly improves patient outcomes in this high-stakes clinical scenario.

