Progressive Familial Intrahepatic Cholestasis (PFIC) is a group of rare, genetically inherited liver disorders characterized by defective bile flow (cholestasis) beginning in infancy or early childhood. One of the most debilitating symptoms experienced by patients with PFIC is pruritus, or chronic itch, often leading to excoriations, sleep disturbances, and severely diminished quality of life. Effective understanding and management of PFIC-related pruritus are essential for improving patient outcomes.

Overview of PFIC: Genetic and Clinical Basis
PFIC includes multiple subtypes, each linked to a specific genetic mutation that disrupts bile secretion mechanisms:
- PFIC type 1 (ATP8B1 gene)
- PFIC type 2 (ABCB11 gene)
- PFIC type 3 (ABCB4 gene)
These subtypes impair hepatocellular bile salt transport, leading to toxic accumulation of bile acids in the liver and systemic circulation.
Pathophysiology of Pruritus in PFIC
The mechanism of pruritus in PFIC is multifactorial, involving:
- Retention of bile acids: Pruritogens such as bile salts accumulate in the bloodstream and dermal tissue.
- Lysophosphatidic acid (LPA): Elevated LPA, produced via autotaxin activity, is strongly linked with chronic itching in cholestasis.
- Opioidergic dysregulation: Imbalance of endogenous opioids enhances itch perception.
Clinical Presentation: Pruritus as a Dominant Symptom
Pruritus in PFIC typically appears within the first months of life and is often more distressing than jaundice or hepatomegaly. Key features include:
- Intense, generalized itching
- Sleep disturbances
- Behavioral irritability in infants
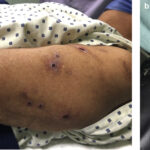
- Excoriations and skin infections
- Lichenification and thickened skin
Patients may not have obvious jaundice, making pruritus a critical clinical clue to underlying PFIC in infants.
Diagnostic Workup for PFIC-Associated Pruritus
Laboratory Investigations
- Elevated serum bile acids: Strongest indicator of intrahepatic cholestasis
- Liver enzymes: GGT levels help differentiate PFIC types (e.g., low in PFIC1/2, high in PFIC3)
- Serum autotaxin activity: Emerging biomarker for cholestatic pruritus
Genetic Testing
- Confirms the diagnosis and subtype of PFIC
- Guides therapeutic decisions, especially for surgical and pharmacologic interventions
Imaging
- Ultrasound and MRCP: Rule out extrahepatic causes of cholestasis
- Liver biopsy: Used selectively to assess fibrosis and histologic subtype
Management of Pruritus in PFIC
First-Line Medical Therapy
- Ursodeoxycholic acid (UDCA): Improves bile flow in some PFIC subtypes
- Cholestyramine: Bile acid sequestrant that binds bile acids in the intestine
- Rifampin: Enhances hepatic excretion and modulates central itch pathways
- Naltrexone: An opioid antagonist to counteract opioid-mediated pruritus
- Antihistamines: Limited role, primarily for sleep support
Advanced Pharmacologic Options
- Ileal bile acid transporter (IBAT) inhibitors: Maralixibat and odevixibat reduce enterohepatic bile acid circulation and have shown promise in clinical trials.
Surgical Interventions
- Partial external biliary diversion (PEBD): Surgically reroutes bile to reduce systemic pruritogen levels, particularly effective in PFIC1 and PFIC2.
- Liver transplantation: Indicated for patients with advanced liver disease or refractory pruritus unresponsive to medical and surgical management.
Quality of Life Considerations
Pruritus significantly impairs health-related quality of life in PFIC patients:
- Poor school performance
- Sleep deprivation
- Social withdrawal
- Emotional distress in caregivers
Routine assessment using validated itch and quality-of-life scales is vital for comprehensive care.
Emerging Therapies and Future Directions
Gene Therapy
- Targeted gene correction strategies are under exploration, offering future curative potential for PFIC-associated symptoms, including pruritus.
FXR Agonists
- Farnesoid X receptor agonists regulate bile acid metabolism and are being studied for cholestatic itch control.
Autotaxin Inhibitors
- Directly reduce LPA levels, thereby targeting a key pruritogenic pathway in cholestasis.
Prognosis and Long-Term Monitoring
Prognosis in PFIC depends on subtype and therapeutic responsiveness:
- PFIC1 and PFIC2: Higher risk for progression to cirrhosis, pruritus often severe
- PFIC3: Slower disease progression, often presents in adolescence
- Regular monitoring: Liver function tests, serum bile acids, and symptom tracking are essential
Pruritus due to progressive familial intrahepatic cholestasis represents a complex clinical challenge, marked by severe and often refractory itching in pediatric populations. A precise understanding of its genetic basis and pathophysiology informs both current and emerging treatment modalities. Through a multidisciplinary approach combining pharmacologic, surgical, and supportive interventions, it is possible to alleviate pruritus, enhance quality of life, and delay progression to end-stage liver disease.