Providencia urinary tract infections (UTIs) are significant contributors to complicated and nosocomial infections, particularly in patients with prolonged catheterization or weakened immunity. Members of the genus Providencia, primarily Providencia stuartii and Providencia rettgeri, are increasingly recognized for their resistance to multiple antibiotics, posing considerable challenges in clinical management.
Overview of Providencia Species and Their Role in UTIs
Microbiological Classification
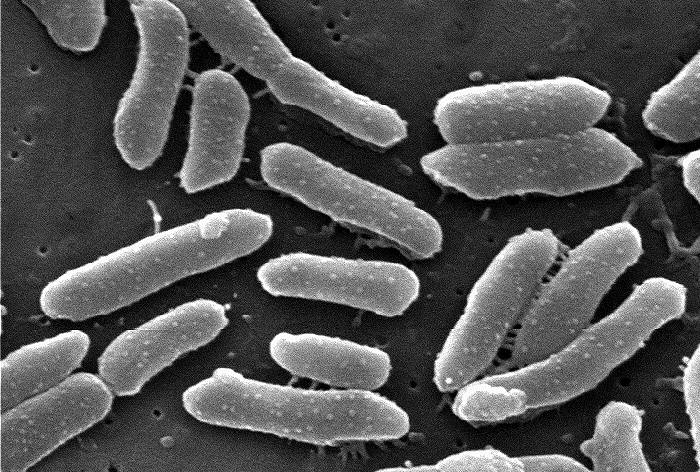
Providencia species are Gram-negative, motile rods within the family Enterobacteriaceae. They are non-lactose fermenters and urease-positive, characteristics that distinguish them in diagnostic microbiology.
Pathogenic Species
- Providencia stuartii: Most frequently implicated in UTIs, especially in catheterized patients.
- Providencia rettgeri: Also causes UTIs and is known for extensive drug resistance.
- Less common species include Providencia alcalifaciens and Providencia rustigianii.
Risk Factors for Providencia-Associated Urinary Tract Infections
Primary Risk Factors
- Long-term indwelling urinary catheters
- Residency in long-term care facilities
- Hospitalization with ICU stay
- Structural abnormalities in the urinary tract
- Neurogenic bladder or spinal cord injury
- Immunocompromised states (e.g., diabetes, malignancy)
Pathogenesis: From Colonization to Infection
Biofilm Formation
Providencia species form robust biofilms on catheter surfaces, protecting them from host defenses and antibiotics. This contributes to persistent infections and reinfection cycles.
Urease Activity
The urease enzyme hydrolyzes urea into ammonia, raising urine pH and precipitating magnesium ammonium phosphate (struvite) crystals. This leads to encrustation, obstruction, and recurrent infections.
Clinical Presentation of Providencia UTI
Common Symptoms
- Dysuria (painful urination)
- Suprapubic pain
- Urgency and frequency
- Foul-smelling urine
- Hematuria (blood in urine)
- Fever, chills in upper urinary tract involvement
Atypical Presentations
- Asymptomatic bacteriuria in elderly or catheterized patients
- Delirium or confusion in geriatric populations
- Septicemia in cases of delayed or untreated infection
Diagnostic Approaches
Urinalysis
- Presence of pyuria (white blood cells)
- Nitrite-positive and alkaline pH suggest urease-producing organisms
- Microscopic hematuria or crystalluria may be present
Urine Culture
- Confirmatory for diagnosis
- Providencia typically shows resistance to first-line antibiotics
- Colony counts >10⁵ CFU/mL with symptoms support diagnosis
Susceptibility Testing
Essential for guiding antibiotic therapy due to high rates of resistance.
Antimicrobial Resistance in Providencia UTIs
Common Resistance Mechanisms
- Extended-spectrum β-lactamases (ESBLs)
- Carbapenemases including NDM-1
- Efflux pumps and decreased porin expression
Resistance Profile
| Antibiotic Class | Resistance Frequency |
|---|---|
| Penicillins | High |
| Cephalosporins | High |
| Carbapenems | Variable to High |
| Fluoroquinolones | Common |
| Aminoglycosides | Moderate |
| Nitrofurantoin | Usually Resistant |
| Fosfomycin | Variable |
Therapeutic Management of Providencia UTIs
Empiric Therapy
Initial treatment should consider local antibiograms and the patient’s clinical status. For severe cases or known ESBL producers:
- Carbapenems (e.g., meropenem, ertapenem)
- Ceftazidime-avibactam for carbapenem-resistant strains
- Aminoglycosides if susceptibility confirmed
- Fosfomycin may be used in selected cases
Definitive Therapy
Refined based on culture and susceptibility results. Treatment duration:
- Uncomplicated UTI: 7–10 days
- Complicated UTI: 10–14 days
- Catheter-associated UTI: Requires device replacement/removal
Preventive Strategies in Healthcare Settings
Catheter-Associated UTI (CAUTI) Reduction
- Minimize duration of catheterization
- Use of closed drainage systems
- Routine catheter care with sterile techniques
- Avoid unnecessary catheterization
Antimicrobial Stewardship
- Avoid empirical overuse of broad-spectrum antibiotics
- De-escalate therapy based on culture
- Implement facility-specific treatment protocols
Surveillance and Infection Control
- Monitor UTI incidence and resistance patterns
- Isolate patients with multidrug-resistant Providencia when necessary
- Staff education on hygiene and infection prevention
Complications of Providencia UTIs
Short-Term Complications
- Pyelonephritis
- Septicemia
- Acute kidney injury
- Struvite stone formation
Long-Term Consequences
- Recurrent infections
- Renal scarring in chronic infections
- Increased antibiotic resistance
- Prolonged hospitalization
Providencia urinary tract infections are a growing challenge in healthcare environments due to their association with long-term catheter use and multidrug resistance. Prompt diagnosis, appropriate antibiotic therapy, and proactive prevention strategies are essential in mitigating complications and improving outcomes. By adopting evidence-based approaches and enhancing awareness among healthcare professionals, we can effectively manage and reduce the burden of Providencia-associated UTIs.

