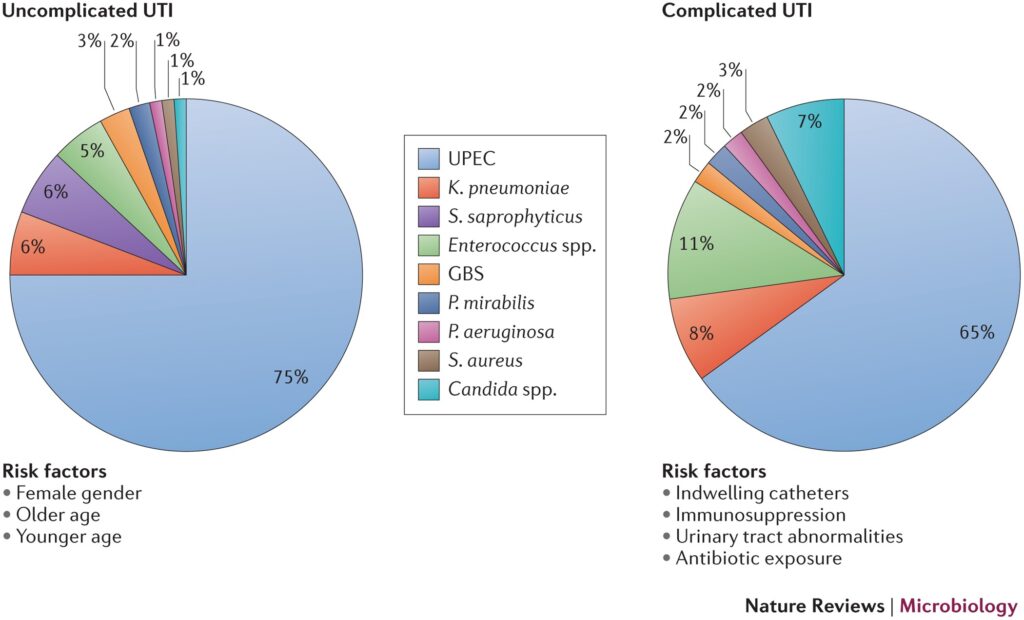
Providencia species, notably Providencia stuartii and Providencia rettgeri, are emerging pathogens responsible for complicated urinary tract infections (UTIs), particularly in healthcare settings. These Gram-negative bacilli pose significant clinical challenges due to their intrinsic resistance mechanisms and association with indwelling medical devices. This article provides a detailed review of Providencia complicated UTIs, from pathophysiology and diagnosis to current treatment and prevention strategies.
Overview of Providencia and Its Clinical Significance
Taxonomy and Characteristics
Providencia is a genus within the Enterobacteriaceae family. The most clinically significant species in complicated UTIs include:
- Providencia stuartii
- Providencia rettgeri
These organisms are urease-positive, non-lactose fermenting, and motile with peritrichous flagella. They are primarily opportunistic pathogens.
Epidemiological Importance
Providencia infections are most frequently encountered in:
- Long-term care facilities
- Hospitalized elderly patients
- Individuals with chronic indwelling catheters
- Patients with recurrent or chronic UTIs
These infections are typically nosocomial, making them a key concern in infection control and antimicrobial stewardship.
Pathophysiology of Providencia-Associated Complicated UTIs
Urease Activity and Stone Formation
Providencia produces urease, which hydrolyzes urea into ammonia, raising urinary pH. This alkalization facilitates the formation of struvite stones, contributing to chronic infections and obstructive uropathy.
Biofilm Formation
Providencia’s ability to form biofilms on catheters and uroepithelial surfaces protects the bacteria from host immune responses and antimicrobial agents, making eradication difficult.
Risk Factors for Providencia Complicated UTI
Patient-Related Factors
- Advanced age
- Immunosuppression (e.g., diabetes, malignancies)
- Neurological disorders affecting bladder function
- History of recurrent UTIs
Iatrogenic and Environmental Factors
- Indwelling urinary catheters, especially prolonged use
- Frequent hospitalization
- Prior or broad-spectrum antibiotic use
- Presence in long-term care facilities
Clinical Manifestations of Complicated UTI Due to Providencia
Local Symptoms
- Dysuria (painful urination)
- Hematuria (blood in urine)
- Foul-smelling or cloudy urine
- Suprapubic or flank pain
Systemic Complications
- Fever and chills
- Altered mental status in elderly patients
- Sepsis and septic shock in advanced cases
- Formation of renal or perinephric abscesses
These infections are often persistent, resistant to standard antibiotics, and prone to recurrence without targeted intervention.
Diagnostic Workup for Providencia Complicated UTI
Laboratory Investigations
- Urine Culture: Key diagnostic tool; Providencia grows as a non-lactose fermenter with characteristic antibiotic resistance.
- Antibiotic Sensitivity Testing: Essential due to multidrug resistance, particularly to beta-lactams and aminoglycosides.
- Urinalysis: Often shows pyuria, bacteriuria, and elevated pH due to urease activity.
Imaging Studies
For suspected stone formation or obstruction:
- Ultrasound or Non-contrast CT scan of the kidneys, ureters, and bladder to evaluate for anatomical complications and calculi.
Antimicrobial Resistance in Providencia UTIs
Resistance Mechanisms
Providencia spp. often exhibit:
- Extended-spectrum beta-lactamase (ESBL) production
- Carbapenem resistance via metallo-beta-lactamases (e.g., NDM-1)
- Efflux pumps and porin loss contributing to aminoglycoside resistance
Common Resistance Profiles
| Antibiotic Class | Resistance Likelihood |
|---|---|
| Penicillins | High |
| Cephalosporins | High |
| Carbapenems | Increasing |
| Fluoroquinolones | Variable |
| Aminoglycosides | High (especially gentamicin) |
| Fosfomycin | Moderate |
| Nitrofurantoin | Intrinsically resistant |
Treatment of Providencia Complicated UTIs
Empirical and Targeted Therapy
Due to widespread resistance, empirical treatment should be guided by local antibiograms, and definitive therapy must be based on susceptibility testing.
Potential Agents:
- Carbapenems (if susceptible): e.g., meropenem, imipenem
- Piperacillin-tazobactam: If ESBL-negative
- Fosfomycin (oral, for uncomplicated cases)
- Colistin or tigecycline: For multi-drug resistant strains
- Ceftazidime-avibactam or ceftolozane-tazobactam: Newer options for resistant isolates
Duration: Typically 10–14 days; extended in cases of stones or abscesses.
Non-Antibiotic Measures
- Catheter replacement or removal
- Surgical removal of stones
- Drainage of abscesses
- Increased hydration to flush bacteria
Preventive Strategies for Healthcare-Associated Providencia UTIs
Infection Control Protocols
- Minimize duration of catheter use
- Aseptic insertion and maintenance techniques
- Routine catheter surveillance
Antimicrobial Stewardship
- Restriction of unnecessary antibiotics
- Regular review of treatment efficacy
- Use of narrow-spectrum agents whenever possible
Resident and Patient Management
- Bladder training in long-term care
- Adequate hydration and hygiene
- Monitoring and early detection protocols in high-risk individuals
Providencia complicated UTIs represent a significant challenge in healthcare settings, particularly among catheterized and immunocompromised individuals. Their ability to produce urease, form biofilms, and resist multiple drug classes demands a comprehensive approach to diagnosis, treatment, and prevention. Tailored antibiotic therapy, rigorous infection control, and proactive catheter management are critical in reducing morbidity and preventing recurrence of this difficult-to-treat infection.