Proteus septicemia is a critical bloodstream infection most commonly caused by Proteus mirabilis, a gram-negative facultative anaerobic bacillus. Although typically associated with urinary tract infections, Proteus species can breach epithelial barriers, enter the bloodstream, and result in systemic inflammatory response syndrome (SIRS), septic shock, and multi-organ dysfunction if not rapidly treated.
Pathogenesis of Proteus Septicemia
Mechanisms of Invasion and Dissemination
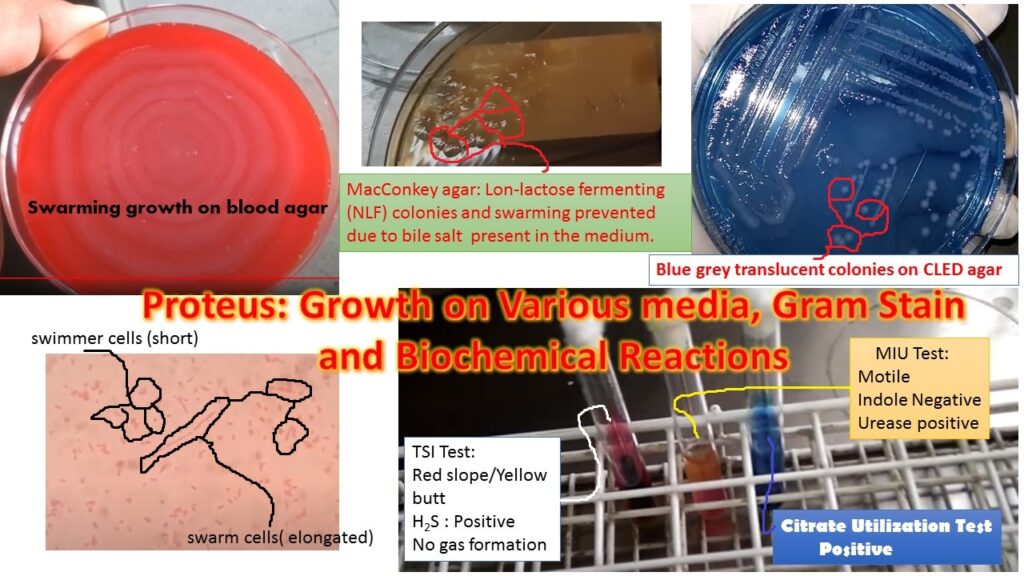
Proteus mirabilis and other species like Proteus vulgaris initiate infection through mucosal colonization, typically of the urinary tract. The progression to septicemia involves:
- Urease production: Leads to ammonia production and alkalization, damaging host tissues.
- LPS endotoxin: Triggers systemic inflammation and cytokine release.
- Hemolysins and proteases: Facilitate tissue destruction and immune evasion.
- Biofilm formation: Enhances resistance to host defenses and antibiotics.
- Flagellar motility: Promotes ascension and tissue invasion.
Risk Factors for Proteus Bloodstream Infections
Patient Profiles with Elevated Susceptibility
- Elderly or immunocompromised individuals
- Patients with indwelling catheters or devices
- Chronic urinary tract infection patients
- Those undergoing recent urological procedures
- Diabetic patients with impaired neutrophil function
- Neonates, especially in intensive care settings
Nosocomial acquisition is common, especially in intensive care units (ICUs), where invasive interventions are prevalent.
Clinical Presentation of Proteus Septicemia
Signs and Symptoms of Systemic Infection
The manifestations are often non-specific initially, but escalate rapidly:
- High-grade fever with rigors and chills
- Hypotension and tachycardia
- Altered mental status or confusion in elderly
- Decreased urine output indicating renal involvement
- Nausea, vomiting, or signs of primary infection source (e.g., flank pain in UTI)
If untreated, it may progress to septic shock, disseminated intravascular coagulation (DIC), and multi-organ failure.
Essential Diagnostic Tools
- Blood cultures: Gold standard for identifying bacteremia.
- Urine or wound cultures: May indicate the source.
- Procalcitonin and CRP: Markers of systemic inflammation.
- Imaging: Ultrasound, CT, or MRI to identify abscesses, stones, or other niduses of infection.
- Complete blood count: Often reveals leukocytosis or leukopenia.
Targeted Antimicrobial Therapy
Empiric and Tailored Regimens
Empiric treatment should begin immediately in suspected cases. Recommended agents include:
- Carbapenems (e.g., meropenem) for ESBL-producing strains
- Piperacillin-tazobactam for broad-spectrum initial therapy
- Third- or fourth-generation cephalosporins (e.g., ceftriaxone, cefepime)
- Fluoroquinolones (e.g., ciprofloxacin) if sensitive
- Aminoglycosides (e.g., gentamicin) may be added in synergistic regimens
Treatment duration: Typically 10–14 days, adjusted based on clinical response and clearance of bacteremia.
Complications of Untreated or Severe Proteus Septicemia
Potential Life-Threatening Outcomes
Without prompt and effective treatment, complications may include:
- Septic shock
- Acute respiratory distress syndrome (ARDS)
- Acute kidney injury (AKI)
- Metastatic abscesses (e.g., liver, spleen)
- Infective endocarditis
- DIC and multiorgan dysfunction syndrome (MODS)
These complications require intensive supportive care and prolonged hospitalization.
Supportive Measures in the Management of Proteus Septicemia
Multidisciplinary Critical Care Approach
- Intravenous fluid resuscitation
- Vasopressors (e.g., norepinephrine) if hypotension persists
- Renal replacement therapy for AKI
- Mechanical ventilation in respiratory failure
- Nutritional and glycemic support for immune modulation
- Source control via drainage or removal of infected devices
Timely involvement of infectious disease specialists is essential for optimal outcomes.
Prevention and Hospital Protocols
Strategies for Infection Control
- Strict aseptic techniques during catheter insertion and care
- Timely removal of unnecessary invasive devices
- Antibiotic stewardship to prevent resistance
- Screening and isolation of colonized patients in high-risk wards
- Prophylactic antibiotics in high-risk urological procedures
Hospitals must maintain stringent infection control measures, especially in ICU and postoperative units.
Proteus septicemia is a dangerous and aggressive bloodstream infection that necessitates immediate attention. With its roots often in urinary tract infections, it rapidly progresses without warning and carries significant mortality if left untreated. Through early diagnosis, aggressive antimicrobial therapy, and appropriate supportive measures, patient outcomes can be significantly improved. Prevention through infection control and surveillance remains pivotal in reducing incidence rates in both community and hospital settings.