Proteus prostatitis is a form of bacterial inflammation of the prostate gland predominantly caused by Proteus mirabilis, a gram-negative bacillus commonly implicated in urinary tract infections. This condition may manifest acutely or chronically and is particularly challenging due to the pathogen’s virulence factors and antibiotic resistance profile. Timely diagnosis and targeted treatment are essential for preventing complications and recurrence.
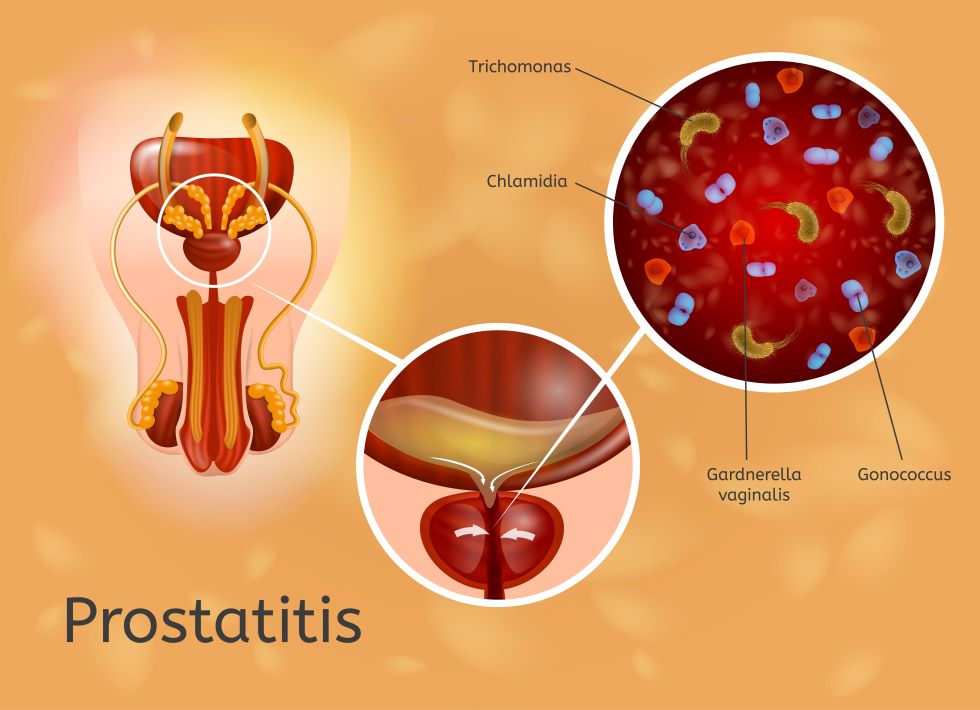
Etiology and Microbiology of Proteus-Induced Prostatitis
Pathogenic Mechanisms of Proteus mirabilis
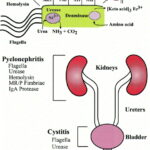
Proteus mirabilis is part of the Enterobacteriaceae family and exhibits several virulence traits that contribute to its pathogenicity in the male urogenital tract:
- Flagella-mediated motility: Facilitates migration through the urethra into the prostate.
- Urease production: Raises local pH, promoting the formation of struvite stones and tissue irritation.
- Biofilm formation: Enhances bacterial persistence and resistance to host defenses and antibiotics.
- Fimbriae (adhesins): Enable firm attachment to uroepithelial surfaces.
These features make Proteus a formidable pathogen in cases of complicated urinary tract infections that ascend to involve the prostate.
Clinical Classification and Risk Factors
Acute vs. Chronic Proteus Prostatitis
Acute bacterial prostatitis typically presents with severe systemic and urinary symptoms, while chronic bacterial prostatitis involves recurring or persistent infection often refractory to treatment.
Predisposing Factors
- Indwelling catheters or intermittent catheterization
- Previous urinary tract infections
- Prostatic hypertrophy or urethral obstruction
- Immunosuppression or poorly controlled diabetes
- History of instrumentation or prostate biopsy
- Incomplete or inappropriate antibiotic therapy
Signs and Symptoms of Proteus Prostatitis
Distinctive Clinical Features
Acute Presentation
- Sudden onset of fever and chills
- Pelvic or perineal pain
- Painful and frequent urination (dysuria, urgency)
- Cloudy or foul-smelling urine
- Painful ejaculation or erectile dysfunction
- Tender, edematous prostate on digital rectal exam (DRE)
Chronic Presentation
- Recurrent urinary tract symptoms
- Low-grade fever
- Chronic pelvic pain syndrome (CPPS)
- Intermittent hematuria or pyuria
- Sterile pyuria with positive prostatic secretion cultures
Diagnostic Workup and Laboratory Investigations
Confirmatory Testing for Proteus Prostatitis
Key Diagnostic Tools
- Urine culture: Midstream or post-prostatic massage specimens may isolate Proteus mirabilis.
- Expressed prostatic secretions (EPS): Collected during DRE and evaluated microscopically.
- Blood tests: Elevated white cell count, ESR, and CRP in acute cases.
- Imaging: Transrectal ultrasound or MRI for abscesses, calcifications, or structural anomalies.
Antimicrobial Therapy and Clinical Management
Empirical and Culture-Guided Treatment
Initial therapy must cover gram-negative organisms until cultures confirm sensitivity. Common choices include:
- Fluoroquinolones (e.g., ciprofloxacin, levofloxacin)
- Trimethoprim-sulfamethoxazole
- Third-generation cephalosporins (e.g., ceftriaxone)
- Aminoglycosides (e.g., gentamicin) in hospitalized patients
Treatment Duration
- Acute prostatitis: 2–4 weeks
- Chronic prostatitis: 4–6 weeks or longer
Adjunctive Therapies
- Alpha-blockers to relieve urinary symptoms
- NSAIDs for pain and inflammation
- Sitz baths and prostatic massage (with caution)
- Surgical drainage for abscesses
Complications and Prognostic Considerations
Long-Term Consequences of Untreated or Refractory Infection
Without appropriate intervention, Proteus prostatitis may lead to:
- Prostatic abscess formation
- Chronic pelvic pain syndrome (CPPS)
- Seminal vesiculitis or infertility
- Epididymitis or orchitis
- Urosepsis, particularly in immunocompromised patients
Early, targeted antimicrobial therapy significantly improves outcomes and reduces the risk of chronicity.
Preventive Strategies and Recurrence Reduction
Measures to Minimize Risk and Reinfection
- Prompt treatment of lower urinary tract infections
- Avoidance of unnecessary catheterization
- Adequate hydration and urinary hygiene
- Prostate-friendly dietary habits and lifestyle modifications
- Regular follow-up and post-treatment cultures to confirm eradication
Antibiotic stewardship and infection control are key in preventing multidrug-resistant Proteus strains.
Proteus prostatitis represents a clinically challenging infection requiring a thorough understanding of the pathogen, host risk factors, and individualized treatment strategies. A high index of suspicion, robust microbiological evaluation, and adherence to prolonged, targeted therapy are fundamental in achieving symptom resolution and preventing recurrence. Proactive management and vigilance are indispensable to combating this persistent form of bacterial prostatitis.