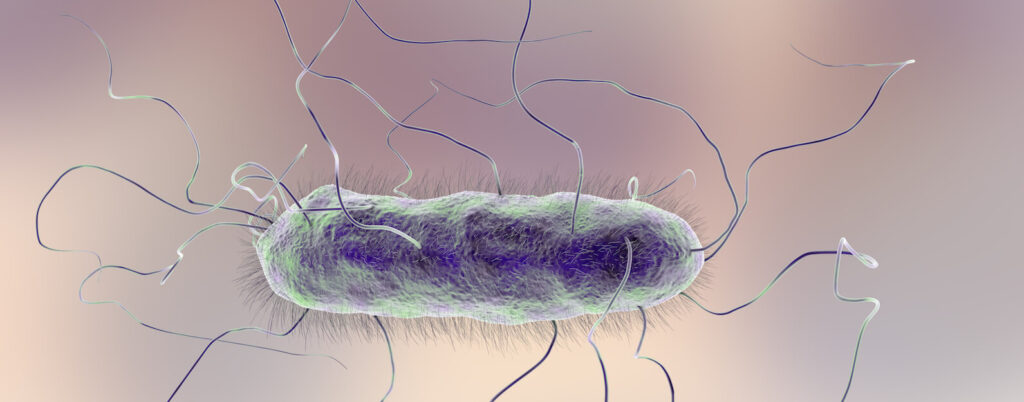
Proteus mirabilis is a gram-negative, facultatively anaerobic bacillus belonging to the Enterobacteriaceae family. Recognized for its urease production and robust motility, it is a prominent cause of complicated urinary tract infections (UTIs), particularly in catheterized individuals, patients with urinary tract abnormalities, or recurrent infections. This article provides a comprehensive, evidence-based analysis of the pathogenesis, clinical features, diagnosis, and management of Proteus mirabilis urinary tract infections.
Pathophysiology of Proteus mirabilis in Urinary Tract Infections
Urease Activity and Stone Formation
One of the defining characteristics of Proteus mirabilis is its potent urease enzyme, which hydrolyzes urea into ammonia and carbon dioxide. This biochemical activity results in urine alkalinization, promoting the formation of struvite (magnesium ammonium phosphate) and apatite stones, and enhances bacterial adherence to the uroepithelium.
Virulence Mechanisms
- Flagella: Allow swarming motility and ascendancy in the urinary tract
- Fimbriae (MR/P, PMF): Facilitate adherence to uroepithelial cells
- Hemolysins and proteases: Cause tissue damage and immune evasion
- Biofilm formation: Especially on indwelling catheters, leading to persistent infections
Risk Factors and Epidemiology
Predisposing Conditions
- Long-term indwelling urinary catheters
- Neurogenic bladder or urinary stasis
- Structural abnormalities such as ureteral strictures
- Recurrent UTIs and prior antibiotic use
- Renal calculi (stone formation)
Populations at Higher Risk
- Elderly individuals
- Hospitalized or institutionalized patients
- Individuals with spinal cord injuries
- Immunocompromised patients (e.g., diabetes, malignancy)
Clinical Manifestations of Proteus mirabilis UTI
Symptom Profile
While the presentation may overlap with typical UTIs, specific signs associated with Proteus mirabilis include:
- Dysuria, urgency, and frequency
- Suprapubic discomfort or pelvic pain
- Foul-smelling, cloudy urine
- Hematuria (blood in urine)
- Flank pain indicating pyelonephritis
- Fever and chills in complicated cases
Complications
- Formation of large renal or bladder stones (struvite)
- Progression to pyelonephritis or urosepsis
- Chronic or recurrent UTIs
- Obstructive uropathy
Diagnostic Evaluation
Laboratory Testing
- Urinalysis: Typically reveals alkaline urine, pyuria, bacteriuria, and sometimes hematuria.
- Urine culture: Confirms Proteus mirabilis and guides antibiotic selection.
- Imaging: Indicated in recurrent infections or when obstruction/stone formation is suspected.
Antimicrobial Management of Proteus mirabilis UTI
First-Line Treatment
- Trimethoprim-sulfamethoxazole: Effective for uncomplicated cases
- Ciprofloxacin or levofloxacin: Preferred for their renal tissue penetration
- Ceftriaxone or cefepime: For inpatient or parenteral therapy
Considerations for Complicated Infections
- Duration: 7–14 days based on severity and site of infection
- Tailoring therapy based on culture sensitivity is essential due to emerging resistance
- Avoid nitrofurantoin and fosfomycin in upper tract involvement due to poor tissue penetration
Management of Recurrent and Catheter-Associated UTIs
Biofilm and Device Management
Biofilms formed by Proteus mirabilis on catheters are resistant to antibiotics and host defenses.
- Regular catheter changes
- Antiseptic-coated catheters
- Removal of unnecessary devices
- Bladder irrigation with non-toxic agents under medical supervision
Suppressive Therapy
May be considered in patients with recurrent infections and non-removable risk factors after evaluating resistance profiles and renal function.
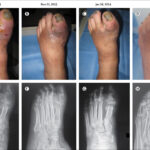
Stone-Related Proteus UTI
When associated with struvite stones, antimicrobial therapy alone is insufficient.
Surgical Intervention
- Percutaneous nephrolithotomy or lithotripsy: For large or obstructive stones
- Stent or nephrostomy placement: In cases of hydronephrosis or urosepsis
- Complete stone removal: Essential to eliminate infection nidus
Prevention Strategies
Infection Control Measures
- Aseptic catheter insertion and maintenance
- Avoid unnecessary catheterization
- Adequate hydration to reduce bacterial adhesion
- Acidification of urine (dietary or pharmacological) under clinical guidance
Prognosis and Outcomes
Favorable Factors
- Prompt diagnosis
- Effective antibiotic therapy
- Elimination of predisposing factors (e.g., catheter removal, stone clearance)
Poor Prognostic Indicators
- Delayed treatment
- Extensive stone burden
- Underlying chronic kidney disease or structural anomalies
- Repeated catheter-associated infections
Proteus mirabilis urinary tract infections, while less prevalent than Escherichia coli, represent a significant clinical challenge due to their association with biofilms, stone formation, and complicated urinary tract involvement. A multifaceted approach encompassing targeted antimicrobial therapy, imaging diagnostics, catheter and stone management, and infection control practices is essential to reduce recurrence and morbidity. Long-term outcomes can be significantly improved through early detection and comprehensive care in susceptible individuals.