Candida pleural space infection is a serious and rare condition that involves the infection of the pleural space by Candida species. This infection, although uncommon, can lead to significant complications if not diagnosed and treated promptly. In this article, we explore the various aspects of Candida pleural space infection, including its causes, symptoms, diagnosis, treatment options, and prevention strategies, providing a comprehensive understanding of this life-threatening condition.
Understanding Candida Pleural Space Infection
What Is Candida Pleural Space Infection?
Its a refers to the presence of Candida species, a type of yeast, within the pleural cavity—the area between the layers of tissue that surround the lungs. This infection is characterized by the infiltration of Candida into the pleural fluid or the pleural lining, potentially leading to a pleural effusion. A pleural effusion occurs when excess fluid accumulates in the pleural space, impairing lung function and leading to difficulty breathing and other severe respiratory symptoms.
Candida species are opportunistic pathogens that typically affect individuals with weakened immune systems, making them more susceptible to fungal infections. In the case of pleural space infections, these microorganisms can enter the pleural cavity through direct extension from neighboring organs, hematogenous spread, or post-surgical complications.
Causes and Risk Factors
Candida infections, including those affecting the pleural space, primarily occur in individuals with compromised immune systems. Some of the common causes and risk factors for Candida pleural space infections include:
- Immune system suppression: Individuals with weakened immune systems due to conditions like HIV/AIDS, cancer, or organ transplants are more prone to fungal infections, including Candida.
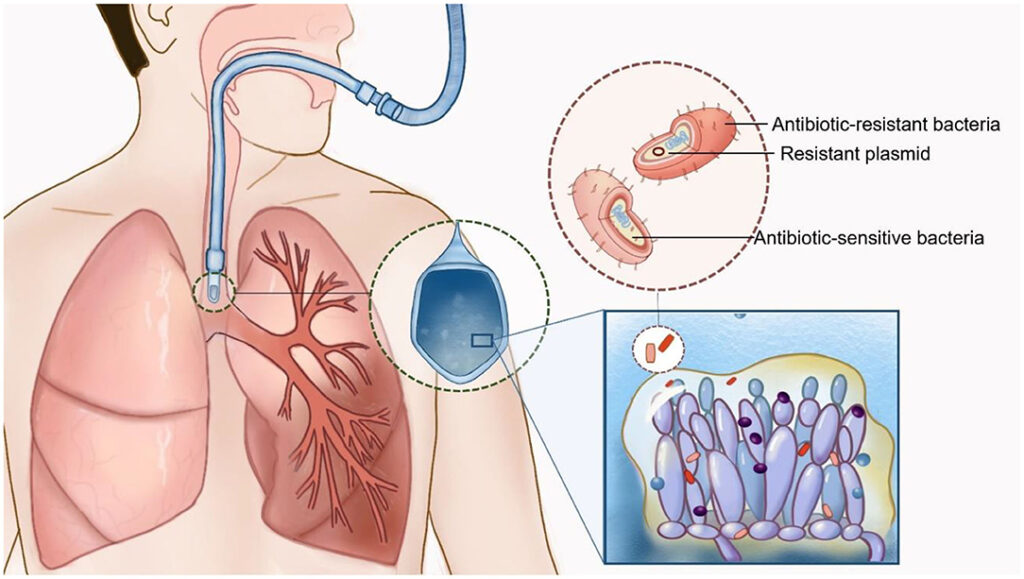
- Post-surgical complications: Procedures such as thoracic surgery or catheter placement can introduce Candida species into the pleural space, leading to infection.
- Chronic diseases: Conditions like diabetes, chronic obstructive pulmonary disease (COPD), and cirrhosis can increase the risk of developing Candida pleural space infections.
- Prolonged antibiotic or corticosteroid use: These medications can alter the balance of microorganisms in the body, making it easier for Candida to proliferate.
- Intravenous drug use: Using intravenous drugs with contaminated needles increases the risk of infection through hematogenous spread.
Symptoms
The symptoms of Candida pleural space infection vary depending on the severity of the infection, the underlying health of the patient, and whether the infection leads to pleural effusion. Common signs and symptoms include:
- Chest pain: This pain is often sharp and may worsen with breathing or coughing, a hallmark symptom of pleural effusion.
- Shortness of breath: Difficulty breathing can result from the accumulation of fluid in the pleural cavity, impairing lung expansion.
- Cough: Persistent coughing may occur, accompanied by mucus production or even blood in severe cases.
- Fever and chills: Systemic symptoms such as fever and chills are often present, reflecting the body’s response to infection.
- Fatigue: As with many infections, Candida pleural space infection can lead to significant fatigue and weakness.
If left untreated, Candida pleural space infections can result in life-threatening complications, such as respiratory failure, sepsis, or the formation of an abscess within the pleural space.
Diagnosis
Diagnosing Candida pleural space infection requires a combination of clinical examination, imaging studies, and microbiological testing. The steps involved in diagnosing this infection include:
Clinical Examination
A thorough clinical examination often reveals signs of pleural effusion, including reduced breath sounds, dullness to percussion, and signs of respiratory distress. Physicians may also observe systemic signs of infection, such as fever and tachycardia.
Imaging Studies
- Chest X-ray: This is the first-line imaging study to detect pleural effusion. A typical finding in Candida pleural space infection is a unilateral pleural effusion, though bilateral effusions can also occur.
- CT scan: A more detailed imaging technique, CT scans help assess the extent of the pleural effusion, the presence of any abscesses, and the overall condition of the lungs and surrounding structures.
- Ultrasound: This can guide the physician in performing thoracentesis (needle aspiration) to obtain pleural fluid for analysis.
Microbiological Testing
Once pleural fluid is obtained through thoracentesis or a biopsy, it is sent for microbiological testing to identify the presence of Candida. Culturing pleural fluid is crucial, as Candida species may not be easily detected with routine bacterial cultures. The fluid may also be tested for its fungal load and for the presence of other pathogens.
Treatment Options
Effective treatment of Candida pleural space infection requires a multidisciplinary approach. The main components of treatment include antifungal therapy, drainage of pleural effusions, and supportive care.
Antifungal Therapy
The cornerstone of treatment for Candida pleural space infection is antifungal therapy. The most commonly used antifungal agents for Candida infections are:
- Echinocandins (e.g., caspofungin, micafungin): These are first-line agents due to their effectiveness against Candida species, particularly in critically ill patients.
- Fluconazole: This is often used for non-severe cases or as a step-down therapy after the patient stabilizes.
- Amphotericin B: In cases of severe infection or resistance to other antifungal treatments, amphotericin B may be used.
Drainage of Pleural Effusion
In cases where pleural effusion is present, the accumulation of fluid needs to be addressed. Thoracentesis or chest tube insertion is performed to remove the excess pleural fluid, relieving pressure on the lungs and improving respiratory function. In some cases, surgical intervention may be required to drain persistent or loculated effusions.
Supportive Care
Supportive care, including oxygen therapy, mechanical ventilation (if needed), and fluid management, is essential for stabilizing patients with severe Candida pleural space infections. Close monitoring in an intensive care unit (ICU) may be required for patients with respiratory distress or sepsis.
Prevention
Providing Candida pleural space infection involves minimizing the risk factors that contribute to infection. Strategies for prevention include:
- Infection control practices: Proper hygiene, including regular hand washing and sterilization of medical equipment, is crucial in preventing fungal infections in healthcare settings.
- Careful antibiotic use: Judicious use of antibiotics can reduce the disruption of normal flora, helping to prevent fungal overgrowth.
- Monitoring immune-compromised patients: Individuals with weakened immune systems should be closely monitored for signs of infection, especially after surgeries or invasive procedures.
- Prophylactic antifungal therapy: For high-risk patients, antifungal prophylaxis may be recommended to prevent Candida infections.
Prognosis and Outlook
The prognosis for patients with this varies depending on the severity of the infection, the underlying health of the patient, and how quickly treatment is initiated. Early detection and aggressive antifungal therapy are crucial in improving outcomes. However, complications such as persistent pleural effusion or sepsis can worsen the prognosis, making timely intervention critical.