Proteus mirabilis, a gram-negative facultative anaerobe, is an opportunistic pathogen increasingly associated with osteomyelitis, particularly in immunocompromised patients and those with chronic wounds, trauma, or prosthetic implants. This article presents a detailed, evidence-based exploration of the pathogenesis, diagnosis, treatment, and surgical interventions relevant to Proteus mirabilis osteomyelitis.

Microbiological Profile and Pathogenesis of Proteus mirabilis in Bone Infections
Key Virulence Mechanisms
Proteus mirabilis exhibits multiple pathogenic traits that contribute to its ability to colonize and damage osseous tissue:
- Urease production: Leads to local alkalinization and crystal deposition.
- Flagella-mediated motility: Facilitates movement through connective tissues.
- Fimbriae and adhesins: Aid in adherence to bone matrix and implant surfaces.
- Biofilm formation: Protects bacteria from immune responses and antimicrobials.
These characteristics promote persistence in bone tissue and resistance to conventional therapies, complicating clinical outcomes.
Epidemiology and Risk Factors
Common Clinical Scenarios
- Post-traumatic open fractures
- Diabetic foot ulcers with underlying osteomyelitis
- Pressure sores in immobilized patients
- Postoperative orthopedic implant infections
- Urinary tract infections with hematogenous spread in immunocompromised individuals
High-Risk Populations
- Elderly patients
- Diabetics with peripheral vascular disease
- Long-term care residents
- Patients with chronic indwelling catheters
Clinical Presentation of Proteus mirabilis Osteomyelitis
Symptoms are often nonspecific but may progress insidiously in chronic forms:
- Localized bone pain, swelling, and warmth
- Erythema or overlying skin ulceration
- Fever and malaise (in acute or systemic infection)
- Non-healing wounds or exposed bone
- Purulent drainage from sinus tracts
Delayed diagnosis is common due to the subtle presentation in chronic cases, particularly in neuropathic limbs.
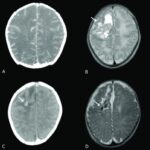
Imaging Modalities
- X-rays: May reveal cortical erosion or periosteal reaction in later stages.
- MRI: Gold standard for early detection; identifies marrow edema and abscess.
- CT and bone scans: Useful in evaluating chronic or complex infections.
Microbiological Confirmation
- Bone biopsy remains the definitive method for identifying Proteus mirabilis and assessing antibiotic susceptibilities.
Antimicrobial Therapy for Proteus mirabilis Osteomyelitis
Initial Empirical Regimen
Treatment begins empirically but must be tailored based on culture results.
- Ceftriaxone or cefepime: Effective first-line agents for gram-negative coverage
- Piperacillin-tazobactam: Broad-spectrum option for polymicrobial infection
- Carbapenems: Reserved for multidrug-resistant strains
- Fluoroquinolones: Good bone penetration but rising resistance is a concern
Duration of Treatment
- Acute osteomyelitis: Minimum 4–6 weeks IV therapy
- Chronic osteomyelitis: 6–12 weeks with potential for oral step-down based on response
- Suppression therapy: Considered when surgical debridement is incomplete
Surgical Management of Bone Involvement
Surgical Indications
- Necrotic or infected bone requiring debridement
- Abscess formation or sinus tracts
- Failure of medical therapy
- Retained infected implants
Surgical Options
- Debridement and curettage: Removal of necrotic bone and infected tissue
- Resection with bone stabilization: In extensive involvement
- Limb-sparing procedures or amputation: For severe, unmanageable infections
- Placement of antibiotic-loaded spacers: Local delivery in infected cavities
Management of Chronic and Recurrent Infections
Proteus mirabilis osteomyelitis often recurs due to biofilm and poor host immunity.
Strategies to Prevent Recurrence
- Complete surgical excision of infected bone
- Extended antibiotic regimens
- Optimizing glycemic control and vascular status
- Regular wound surveillance in at-risk populations
Adjuvant Therapies
- Negative pressure wound therapy (NPWT)
- Hyperbaric oxygen therapy in selected refractory cases
- Novel antibiofilm agents under investigation
Complications and Prognosis
Potential Complications
- Chronic draining sinus formation
- Pathologic fractures
- Septicemia or endocarditis
- Joint involvement with secondary septic arthritis
- Limb length discrepancy in pediatric patients
Prognostic Determinants
- Timeliness of intervention
- Adequacy of surgical debridement
- Microbial resistance profile
- Host immune status and comorbidities
Prevention and Infection Control
Preventive strategies in high-risk patients and surgical settings are essential.
Preventive Measures
- Preoperative screening and decolonization
- Strict aseptic techniques during orthopedic procedures
- Perioperative antibiotic prophylaxis tailored to local flora
- Management of urinary tract infections before invasive procedures
- Early intervention in diabetic foot infections and pressure ulcers
Proteus mirabilis osteomyelitis, while less frequently encountered than infections caused by staphylococci, poses significant challenges due to its resistance mechanisms and biofilm-forming capacity. Accurate diagnosis, targeted antimicrobial therapy, and definitive surgical intervention remain the pillars of successful management. A multidisciplinary approach involving infectious disease specialists, orthopedic surgeons, and wound care experts is critical to optimizing patient outcomes and reducing recurrence in this complex bone infection.