Proteus meningitis is a rare but severe form of bacterial meningitis predominantly caused by Proteus mirabilis, a gram-negative bacillus. This condition is associated with high morbidity and mortality, particularly among neonates, immunocompromised individuals, and patients with neurosurgical interventions. Prompt recognition and appropriate antimicrobial therapy are crucial for favorable outcomes.
Etiology and Pathogenesis
Proteus mirabilis is a facultative anaerobic gram-negative bacillus belonging to the Enterobacteriaceae family. It is commonly found in the human gastrointestinal tract and the environment. The organism’s virulence factors include swarming motility, urease production, and the ability to form biofilms, facilitating colonization and infection of the urinary tract and, less commonly, the central nervous system (CNS) .
In CNS infections, Proteus species can reach the meninges through hematogenous spread, contiguous extension from adjacent infections, or direct inoculation during neurosurgical procedures. The organism’s ability to produce extended-spectrum beta-lactamases (ESBLs) contributes to its resistance to multiple antibiotics, complicating treatment .
Epidemiology
Proteus meningitis is an uncommon cause of bacterial meningitis. It has been reported in various populations, including neonates, adults with underlying conditions, and post-neurosurgical patients. The incidence is higher among individuals with risk factors such as:
- Neonatal age group
- Immunocompromised states (e.g., HIV infection)
- Neurosurgical interventions
- Urinary tract abnormalities
A study reported Proteus mirabilis as responsible for 4% of gram-negative bacterial meningitis cases over a 21-year period in an American center .
Clinical Presentation
The clinical manifestations of Proteus meningitis are similar to other forms of bacterial meningitis but may vary depending on the patient’s age and immune status. Common symptoms include:
- Fever
- Headache
- Neck stiffness
- Altered mental status
- Seizures
- Vomiting
In neonates, signs may be nonspecific, such as poor feeding, lethargy, irritability, and bulging fontanelle .
Diagnostic Evaluation
Prompt diagnosis is essential for effective management. The diagnostic workup includes:
- Lumbar Puncture: Analysis of cerebrospinal fluid (CSF) typically reveals elevated white blood cell count with neutrophilic predominance, decreased glucose, and elevated protein levels.
- CSF Culture: Isolation of Proteus species confirms the diagnosis.
- Blood Cultures: May also yield the organism, supporting the diagnosis.
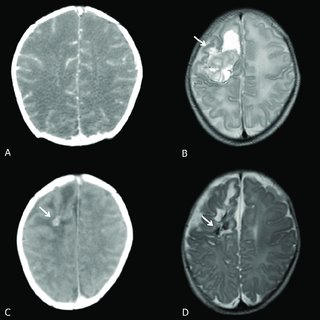
- Neuroimaging: Computed tomography (CT) or magnetic resonance imaging (MRI) may be necessary to assess for complications such as abscess formation .
Treatment Strategies
Management of Proteus meningitis involves prompt initiation of appropriate antimicrobial therapy and supportive care.
Empirical Antimicrobial Therapy
Empirical treatment should cover gram-negative organisms, including ESBL-producing strains. Recommended antibiotics include:
- Third-generation cephalosporins (e.g., ceftriaxone)
- Carbapenems (e.g., meropenem) for ESBL-producing strains
- Aminoglycosides (e.g., amikacin) in combination therapy
Therapy should be adjusted based on culture sensitivities.
Duration of Therapy
The optimal duration of antibiotic therapy is not well established but generally ranges from 21 to 42 days, depending on the patient’s clinical response and presence of complications .
Adjunctive Therapies
In cases with complications such as brain abscesses or hydrocephalus, surgical interventions like abscess drainage or ventriculoperitoneal shunting may be necessary .
Prognosis
The prognosis of Proteus meningitis varies depending on factors such as patient age, immune status, promptness of treatment, and presence of complications. Delayed diagnosis and treatment are associated with higher morbidity and mortality rates. Neonates and immunocompromised individuals are at increased risk for adverse outcomes .
Prevention and Infection Control
Preventive measures are crucial, especially in healthcare settings, to reduce the risk of Proteus meningitis. Strategies include:
- Strict adherence to aseptic techniques during invasive procedures
- Proper sterilization of medical equipment
- Hand hygiene compliance among healthcare workers
- Surveillance and isolation protocols for patients with ESBL-producing organisms
Proteus meningitis, though rare, poses significant clinical challenges due to its potential severity and antibiotic resistance patterns.