Proteus joint infections, though relatively uncommon compared to other causative agents, represent a serious clinical challenge, particularly in cases of prosthetic joint implantation or compromised host immunity. Proteus mirabilis, a motile, urease-producing gram-negative bacillus, is the predominant species implicated. Its capacity for biofilm formation and multidrug resistance necessitates a robust, evidence-based approach to diagnosis and management.
Pathophysiology of Proteus-Induced Joint Infections
Microbial Characteristics and Virulence
Proteus mirabilis thrives in alkaline environments and possesses multiple virulence factors:
- Urease activity: Elevates local pH, disrupting host tissue integrity
- Flagellar motility: Facilitates deep tissue invasion
- Fimbriae and adhesins: Enhance colonization of synovial tissues and implants
- Biofilm formation: Shields bacteria from immune responses and antibiotics
In prosthetic joint infections (PJI), biofilm formation on implant surfaces severely hampers eradication efforts, leading to chronic, relapsing infections.
Clinical Risk Factors and Patient Populations
Predisposing Conditions
- Prosthetic joint implants (especially hip and knee arthroplasties)
- Recent orthopedic surgeries
- Open fractures or penetrating joint trauma
- Diabetes mellitus and immunocompromised states
- Chronic urinary tract infections (hematogenous spread)
- Indwelling urinary catheters or long-term care facility residence
These conditions heighten vulnerability by either providing microbial access to joint spaces or impairing host immune defenses.
Signs and Symptoms of Proteus Joint Infections
Acute Septic Arthritis
- Rapid onset of joint pain, swelling, and erythema
- Fever, chills, and systemic signs of sepsis
- Restricted range of motion in the affected joint
- Warmth and effusion on physical examination
Chronic Prosthetic Joint Infection
- Persistent low-grade pain or joint instability
- Sinus tract formation or purulent discharge
- Delayed wound healing after joint replacement
Diagnostic Workflow for Proteus Joint Infection
Effective diagnosis requires integration of clinical suspicion, laboratory data, and imaging studies.
Synovial Fluid Analysis
- Appearance: Turbid or purulent
- WBC count: >50,000 cells/mm³ with PMN predominance
- Gram stain: May reveal gram-negative rods
- Culture: Growth of Proteus mirabilis confirms diagnosis
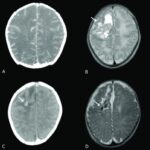
Imaging Modalities
- X-rays may show joint space narrowing or prosthetic loosening
- MRI provides soft tissue resolution for abscess or osteomyelitis
- Tagged white blood cell scans aid in chronic infection detection
Antimicrobial Management of Proteus Joint Infections
Initial Empirical Therapy
Prompt initiation of broad-spectrum intravenous antibiotics is critical, followed by targeted therapy once cultures confirm Proteus species.
Recommended Agents
- Ceftriaxone or Cefepime: Gram-negative coverage
- Piperacillin-tazobactam: If polymicrobial infection is suspected
- Carbapenems: For multidrug-resistant strains
- Avoid aminoglycosides in elderly or renal impairment unless required
Duration of Therapy
- Native joint infections: 2–4 weeks IV, followed by 2–4 weeks oral
- Prosthetic joint infections: 6 weeks IV, potential chronic suppressive therapy if implant retained
Surgical Intervention and Prosthetic Joint Management
Indications for Surgery
- Failure of medical therapy
- Large joint effusion or abscess
- Mechanical instability of prosthesis
- Biofilm-mediated persistent infection
Surgical Options
- Debridement and implant retention (DAIR): For early infections (<3 weeks)
- One-stage exchange arthroplasty: For selected patients
- Two-stage revision surgery: Gold standard for chronic PJI
- Arthrodesis or resection arthroplasty: In non-ambulatory or high-risk patients
Challenges in Eradicating Biofilm-Associated Proteus Infections
Proteus exhibits high resistance within biofilm environments, leading to persistent low-grade infections and poor antibiotic penetration.
Biofilm Disruption Strategies
- Use of rifampin in biofilm-active combinations (not as monotherapy)
- Local delivery systems (e.g., antibiotic-impregnated cement spacers)
- Phage therapy and novel anti-biofilm agents under investigation
Long-Term Outcomes and Prognosis
Factors Influencing Prognosis
- Early and accurate diagnosis
- Complete surgical debridement
- Appropriate antimicrobial selection
- Comorbidity management
Potential Complications
- Joint stiffness or ankylosis
- Recurrent infection
- Functional disability
- Septicemia in untreated cases
Prevention of Proteus Joint Infections in Orthopedic Surgery
Preventive protocols significantly reduce the incidence of Proteus-related infections in prosthetic and native joints.
Prophylactic Measures
- Preoperative skin and urinary tract screening
- Short-term perioperative antibiotic prophylaxis
- Strict aseptic surgical techniques
- Postoperative wound surveillance and early catheter removal
Proteus joint infections, although less common, demand high clinical vigilance due to their aggressive behavior, biofilm resilience, and resistance profile. A multidisciplinary strategy encompassing precise microbiological identification, targeted antibiotic therapy, and individualized surgical management ensures optimal outcomes in both native and prosthetic joint infections. By refining diagnostic approaches and leveraging preventive strategies, we can significantly mitigate the morbidity associated with this formidable pathogen.