Prosthetic heart valve endocarditis (PVE) remains a severe and potentially life-threatening condition in cardiology and cardiac surgery. Despite advancements in valve technology and antibiotic prophylaxis, it presents with high morbidity and mortality. We examine the etiology, pathophysiology, diagnosis, and current therapeutic strategies surrounding PVE, integrating current best practices and innovations.
Overview of Prosthetic Valve Endocarditis
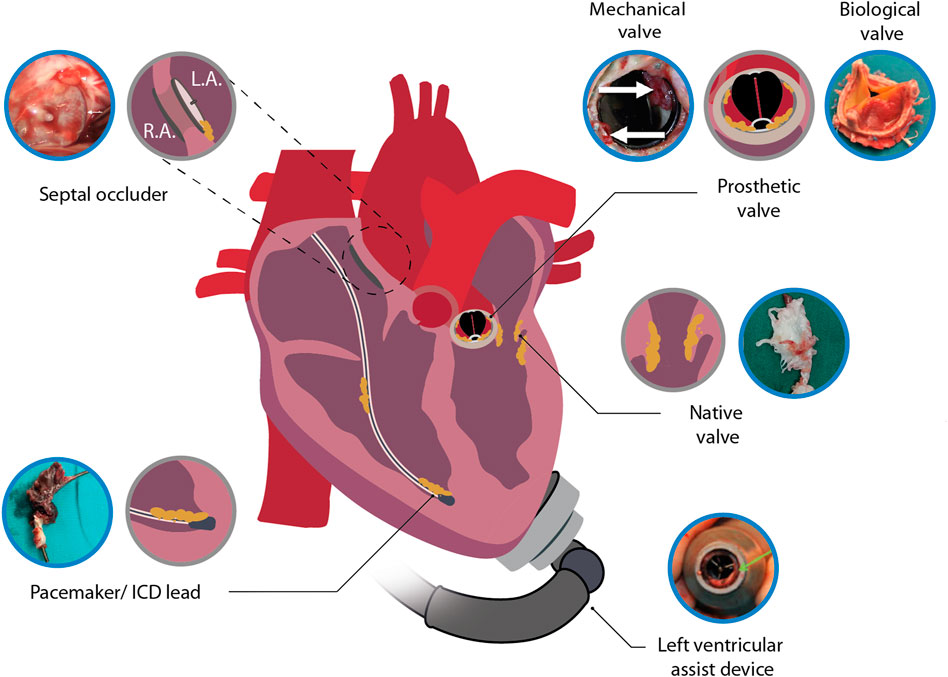
PVE is a subtype of infective endocarditis (IE) that occurs on implanted prosthetic cardiac valves or materials. It is classified based on the timing post-surgery:
- Early-onset PVE: Occurs within 60 days post-implantation.
- Late-onset PVE: Occurs beyond 60 days after surgery.
Incidence and Mortality
- Incidence: 0.3%–1.2% per patient-year post-valve replacement
- Mortality: 20%–40%, depending on timing and complications
Etiology and Microbial Pathogens
Microbial causes differ between early and late PVE:
Common Pathogens
| Timing | Organisms Involved |
|---|---|
| Early | Staphylococcus aureus, CoNS, Gram-negatives |
| Late | Streptococcus spp., Enterococcus spp. |
Coagulase-negative staphylococci (CoNS) are prevalent due to biofilm formation on prosthetic material, making treatment challenging.
Pathogenesis and Mechanisms of Infection
PVE results from microbial seeding of the prosthetic surface, typically via:
- Intraoperative contamination
- Hematogenous spread from distant infections (e.g., dental, urinary)
- Biofilm formation, leading to resistance against host defenses and antibiotics
Clinical Presentation and Diagnostic Features
Symptoms
- Fever, chills, night sweats
- Fatigue, malaise, weight loss
- Heart murmurs or heart failure symptoms
Diagnostic Tools
Duke Criteria (Modified)
- Major: Positive blood cultures, echocardiographic evidence
- Minor: Fever, vascular/immunologic phenomena, predisposing heart condition
Imaging Modalities
- Transesophageal echocardiography (TEE): Gold standard for prosthetic valve assessment
- 18F-FDG PET/CT: Detects infection foci and prosthetic inflammation
- Cardiac CT: Evaluates abscess, pseudoaneurysm, or dehiscence
Antimicrobial Management of Prosthetic Valve Endocarditis
Empiric and pathogen-specific regimens are essential. Treatment duration typically ranges from 6 to 8 weeks.
Empiric Therapy
- Vancomycin + gentamicin + rifampin for early PVE
- Adjust based on organism susceptibility
Pathogen-Specific Therapy
| Organism | First-Line Treatment |
|---|---|
| MSSA | Nafcillin/oxacillin + rifampin + gentamicin |
| MRSA | Vancomycin + rifampin + gentamicin |
| CoNS | Vancomycin or daptomycin + rifampin + gentamicin |
| Enterococcus spp. | Ampicillin + gentamicin or vancomycin-based regimens |
| HACEK organisms | Ceftriaxone |
Surgical Indications and Management
Surgery is often required in up to 50% of PVE cases. Timely intervention improves survival, especially in:
- Heart failure due to valve dysfunction
- Uncontrolled infection
- Prosthetic dehiscence or abscess
- Fungal or resistant infections
Procedures:
- Valve replacement (mechanical or bioprosthetic)
- Debridement of infected tissue
- Repair of annular defects
Prevention Strategies for PVE
Preoperative Measures
- Screen and treat dental infections
- Minimize operative time and reduce intraoperative contamination
Antibiotic Prophylaxis Guidelines (AHA/ESC)
Recommended for high-risk patients undergoing:
- Dental procedures involving manipulation of gingival tissue
- Invasive respiratory or GI procedures in infected individuals
Typical Regimen: Amoxicillin 2 g orally 30–60 min before procedure
Alternative for allergies: Clindamycin 600 mg orally
Long-Term Monitoring and Follow-Up
Post-treatment surveillance includes:
- Regular echocardiographic evaluation
- Monitoring of inflammatory markers (CRP, ESR)
- Clinical assessment for recurrent symptoms
Late recurrence is uncommon with proper treatment and follow-up.
Prosthetic heart valve endocarditis demands an aggressive, multidisciplinary approach involving prompt diagnosis, microbiologically guided antibiotic therapy, and surgical intervention when warranted. Prevention remains vital through appropriate prophylaxis and patient education. Advances in imaging and biofilm-targeted therapies offer promising avenues for improving patient outcomes.