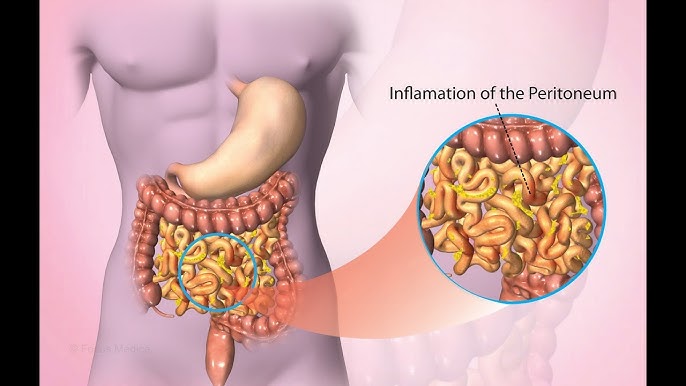
Candida peritonitis is a severe and often life-threatening infection that affects the peritoneum, the thin membrane lining the abdominal cavity and covering the abdominal organs. This condition occurs when Candida, a genus of fungi, invades the peritoneal cavity, causing inflammation and infection. Candida albicans is the most common causative organism, but other Candida species can also contribute to this infection.
In this article, we explore the causes, symptoms, diagnosis, treatment, and prevention of Candida peritonitis, providing healthcare professionals and individuals with the essential knowledge to manage this serious condition.
What is Candida Peritonitis?
Candida peritonitis is a rare but serious infection of the peritoneal cavity. It is most often seen in individuals with compromised immune systems or those who have undergone abdominal surgeries, including peritoneal dialysis or gastrointestinal procedures. The infection occurs when Candida species, which are normally present in the human body, overgrow and invade areas where they are not typically found.
Causes of Candida Peritonitis
The most common cause of Candida peritonitis is the translocation of Candida from the gastrointestinal tract into the peritoneal cavity. This can happen in a variety of scenarios:
- Abdominal Surgery: Surgical procedures such as appendectomy, cholecystectomy, and bowel resections can increase the risk of Candida peritonitis. The introduction of foreign objects like catheters or surgical instruments during these procedures can provide a pathway for Candida to enter the peritoneal cavity.
- Peritoneal Dialysis: Peritoneal dialysis is a well-established treatment for patients with chronic kidney disease. However, it can serve as a gateway for Candida species to infect the peritoneal cavity due to the prolonged exposure of the abdominal cavity to potentially contaminated dialysate.
- Fungal Overgrowth: Patients with compromised immune systems, such as those undergoing chemotherapy, organ transplantation, or suffering from HIV/AIDS, are at increased risk of fungal infections, including Candida peritonitis. The normal immune defense mechanisms are often inadequate to control the overgrowth of Candida in the gastrointestinal tract.
- Gastrointestinal Infections: Conditions like Crohn’s disease or diverticulitis may promote an environment where Candida can proliferate, potentially leading to peritoneal involvement if the infection spreads.
Symptoms of Candida Peritonitis
The symptoms of Candida peritonitis can vary depending on the severity of the infection and the patient’s overall health. Early symptoms often resemble those of bacterial peritonitis, which makes it challenging to diagnose without appropriate testing.
Common symptoms include:
- Abdominal Pain: The most prominent symptom, typically diffuse and crampy, but sometimes localized.
- Abdominal Tenderness and Swelling: The abdomen may become distended, with noticeable tenderness upon palpation.
- Fever and Chills: These are common systemic responses to infection.
- Nausea and Vomiting: Due to the inflammatory response and gastrointestinal upset.
- Altered Bowel Movements: Diarrhea or constipation can occur as a result of peritoneal involvement.
- Signs of Sepsis: In severe cases, Candida peritonitis may progress to septic shock, leading to symptoms like low blood pressure, tachycardia, and organ failure.
Diagnosis
Diagnosing Candida peritonitis can be a challenge due to the nonspecific nature of its symptoms. However, healthcare providers typically rely on a combination of clinical assessment, microbiological cultures, and imaging studies to confirm the diagnosis.
Clinical Assessment
A thorough physical examination and a detailed patient history are essential for diagnosing Candida peritonitis. Factors such as recent abdominal surgery, peritoneal dialysis, or the presence of underlying conditions like diabetes or immunosuppression are key to identifying at-risk patients.
Microbiological Testing
The definitive diagnosis of Candida peritonitis is made through microbiological cultures. A sample of peritoneal fluid, obtained via paracentesis or during surgery, is cultured to identify the presence of Candida species. Blood cultures may also be taken to detect systemic spread of the infection.
Candida species can be identified through a range of laboratory techniques, including:
- Gram Staining: Candida appears as gram-positive, budding yeast cells under the microscope.
- Culture and Identification: Culturing the peritoneal fluid or blood can help determine the exact species of Candida causing the infection.
- Fungal Biomarker Detection: PCR and other advanced molecular methods can identify Candida DNA, although these methods are not commonly used in routine clinical practice.
Imaging Studies
Imaging, such as abdominal X-rays, ultrasounds, or CT scans, may be used to assess the extent of the infection. A CT scan can reveal fluid collections in the peritoneal cavity or signs of perforation, which are indicative of Candida peritonitis.
Treatment of Candida Peritonitis
The treatment of Candida peritonitis typically involves antifungal therapy, supportive care, and, in some cases, surgical intervention. The approach depends on the severity of the infection, the underlying health of the patient, and the specific Candida species involved.
Antifungal Therapy
The first line of treatment for Candida peritonitis is the administration of antifungal medications. Commonly used antifungals include:
- Fluconazole: Often the drug of choice for Candida albicans infections. It can be administered orally or intravenously.
- Echinocandins (Caspofungin, Micafungin, Anidulafungin): These are used for more severe infections or infections caused by non-albicans species, which may be resistant to fluconazole.
- Amphotericin B: This is considered a second-line option for severe or refractory cases of Candida peritonitis, especially in immunocompromised patients.
Treatment duration typically ranges from two to six weeks, depending on the severity of the infection and the patient’s response to therapy. In cases of systemic fungal spread or septic shock, intravenous antifungal therapy is preferred.
Surgical Intervention
Surgical intervention may be necessary if there is a perforation of the gastrointestinal tract, an abscess formation, or a significant peritoneal fluid collection. In these cases, a surgeon may perform:
- Laparotomy or Laparoscopy: To drain infected fluid, repair any perforations, and remove infected tissue if necessary.
- Peritoneal Dialysis Adjustment: For patients undergoing peritoneal dialysis, the dialysate may need to be changed, or the catheter may need to be removed.
Supportive Care
Supportive care is essential in managing Candida peritonitis. This may include:
- Fluid Resuscitation: To treat dehydration, restore electrolyte balance, and stabilize blood pressure.
- Nutritional Support: As patients with peritonitis may be unable to eat normally, nutritional support through enteral or parenteral feeding may be necessary.
- Sepsis Management: If the infection leads to septic shock, intensive care support may be required, including vasopressors and mechanical ventilation.
Prevention of Candida Peritonitis
Preventing Candida peritonitis involves addressing the risk factors and taking proactive measures to minimize exposure to Candida species.
Infection Control in Healthcare Settings
Proper infection control practices, especially in hospitals, are crucial in preventing Candida infections. This includes maintaining sterile techniques during abdominal surgeries, peritoneal dialysis procedures, and catheter insertions.
Appropriate Antifungal Prophylaxis
For high-risk patients, such as those undergoing abdominal surgery or peritoneal dialysis, antifungal prophylaxis may be considered to prevent the onset of Candida peritonitis.
Optimizing Immune Function
Managing underlying conditions, such as diabetes, and providing appropriate treatment for immunocompromised patients can help prevent Candida overgrowth. Regular monitoring for early signs of infection is essential in at-risk populations.