Proctitis is an inflammatory condition of the rectum, characterized by swelling and irritation. It can be caused by a variety of factors, including infections, inflammatory bowel disease (IBD), and radiation therapy. The condition is often painful, and its symptoms can significantly impact the quality of life of those affected. In this article, we will explore the causes, symptoms, diagnostic methods, and treatment options for proctitis, providing an in-depth understanding of this disorder.
What is Proctitis?
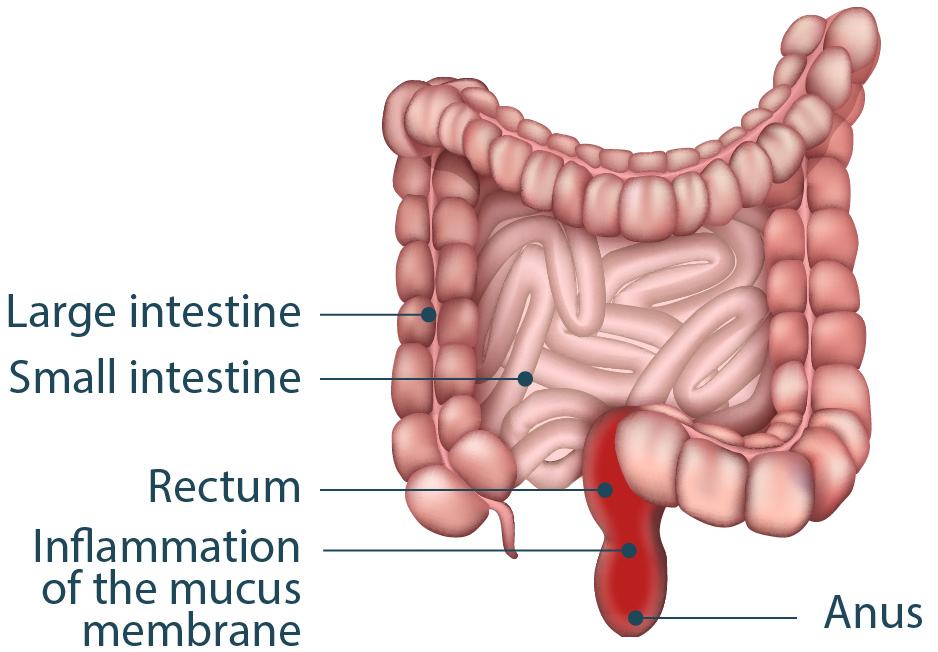
Proctitis refers to inflammation of the inner lining of the rectum. The rectum is the final portion of the large intestine, where stool is stored before being excreted through the anus. Proctitis can manifest as acute or chronic, depending on the underlying cause. The condition may result from various factors, including infections, autoimmune disorders, radiation therapy, and certain medications.
The inflammation can cause pain, discomfort, bleeding, and changes in bowel movements, all of which can significantly affect daily life.
Causes of Proctitis
1. Infectious Proctitis
Infectious proctitis is caused by bacterial, viral, or parasitic infections. Common culprits include:
- Bacterial infections: Neisseria gonorrhoeae, Chlamydia trachomatis, and Treponema pallidum (syphilis) can cause rectal inflammation.
- Viral infections: Herpes simplex virus and human papillomavirus (HPV) are also known to lead to proctitis, particularly in individuals with compromised immune systems.
- Parasitic infections: Protozoa, such as Entamoeba histolytica, and other parasites can trigger proctitis in some cases.
2. Inflammatory Bowel Disease (IBD)
Proctitis is commonly associated with inflammatory bowel diseases, including:
- Ulcerative Colitis: A subtype of IBD that primarily affects the colon and rectum, ulcerative colitis can lead to continuous inflammation and ulcers in the rectal lining.
- Crohn’s Disease: Although Crohn’s disease primarily affects the small intestine and colon, it can also cause proctitis when it extends to the rectum.
In these cases, proctitis is often part of the larger inflammatory process associated with IBD, resulting in chronic inflammation.
3. Radiation Proctitis
Radiation therapy used to treat cancers in the pelvic region, such as prostate or rectal cancer, can lead to radiation-induced proctitis. This type of proctitis occurs due to the damaging effects of radiation on the tissues of the rectum. Radiation proctitis can develop shortly after treatment or months to years later, manifesting as acute or chronic symptoms.
4. Medication-Induced Proctitis
Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, and chemotherapy agents, can irritate the rectal lining and lead to proctitis. This is often a side effect of treatment rather than a direct cause.
5. Allergic Proctitis
Allergic reactions, though rare, can sometimes trigger proctitis. These reactions may be due to food allergies, medication allergies, or sensitivity to other substances.
Symptoms of Proctitis
The symptoms of proctitis vary depending on the underlying cause and whether the condition is acute or chronic. Common symptoms include:
- Rectal pain or discomfort: A sensation of fullness or pain in the rectum, often worsened during bowel movements.
- Rectal bleeding: Bright red blood in the stool or on the toilet paper.
- Diarrhea or constipation: Changes in bowel habits, including frequent diarrhea or difficulty passing stool.
- Mucus discharge: Presence of mucus in the stool.
- Urgency and incontinence: A feeling of needing to urgently pass stool, sometimes leading to accidents.
- Fatigue and fever: In some cases, particularly with infections, general malaise and fever may accompany the symptoms.
In cases of chronic proctitis, these symptoms can persist and fluctuate, requiring long-term management.
Diagnosis of Proctitis
Accurate diagnosis of proctitis requires a thorough medical history and a series of diagnostic tests to identify the underlying cause.
1. Physical Examination
A physical examination typically begins with a digital rectal exam to assess for tenderness, masses, or signs of inflammation in the rectum.
2. Endoscopy
An important diagnostic tool for proctitis is sigmoidoscopy or colonoscopy, which allows a physician to directly visualize the rectal lining and assess the extent of inflammation. During this procedure, tissue samples (biopsies) may be taken for further examination.
3. Laboratory Tests
- Stool cultures and PCR testing can help identify infections caused by bacteria, viruses, or parasites.
- Blood tests may reveal elevated markers of inflammation, such as C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR).
- Serologic tests for autoimmune diseases or sexually transmitted infections (STIs) may also be necessary.
4. Imaging
In some cases, CT scans or MRI scans may be used to assess the extent of inflammation or to rule out other potential causes, such as tumors or abscesses.
Treatment of Proctitis
The treatment of proctitis depends on the underlying cause and the severity of the symptoms.
1. Antibiotics or Antivirals
For infectious proctitis, appropriate antibiotics or antivirals are prescribed to treat bacterial or viral infections. In cases of sexually transmitted infections (STIs), specific therapies for gonorrhea, chlamydia, or herpes simplex virus may be necessary.
2. Anti-Inflammatory Medications
For proctitis associated with inflammatory bowel disease (IBD), aminosalicylates or corticosteroids may be used to reduce inflammation. In more severe cases, immunosuppressive drugs or biologic therapies such as TNF inhibitors may be prescribed to manage chronic inflammation.
3. Radiation Proctitis Management
Treatment for radiation proctitis may include sucralfate enemas, 5-ASA (mesalamine) rectal treatments, or corticosteroids to reduce inflammation. In severe cases, hyperbaric oxygen therapy may be considered to promote healing.
4. Symptom Management
- Pain relief: Nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen can help alleviate pain.
- Fiber supplements or stool softeners may help manage constipation or diarrhea associated with proctitis.
In chronic cases, long-term follow-up with a gastroenterologist is often necessary for symptom management and to monitor for complications.
Prevention of Proctitis
While some forms of proctitis, such as those resulting from radiation or genetic factors, cannot be prevented, the following measures can reduce the risk:
- Safe sex practices: Using condoms and undergoing regular STI screenings can prevent infectious causes of proctitis.
- Management of inflammatory bowel disease: Proper treatment and monitoring of IBD can help prevent flare-ups of proctitis.
- Avoidance of irritants: Limiting the use of irritating medications or substances that can trigger allergic reactions may help in some cases.
Proctitis, though often a manageable condition, can significantly affect a patient’s quality of life if left untreated. Understanding its various causes, symptoms, and available treatments is crucial for effective management. Whether infectious, inflammatory, or radiation-induced, early diagnosis and targeted treatment can help alleviate symptoms and improve outcomes for individuals with proctitis.