Primary malignant neoplasms of the gastrointestinal (GI) tract refer to cancers originating within the various sections of the GI system, which includes the esophagus, stomach, small intestine, colon, rectum, liver, and pancreas. These malignancies represent a major global health burden and are among the leading causes of cancer-related mortality worldwide. Early detection and prompt intervention are critical for improving prognosis and survival rates.
Epidemiology and Risk Factors
Global Prevalence
Gastrointestinal cancers vary in prevalence by region, with colorectal, gastric, and liver cancers among the most frequently diagnosed worldwide. Colorectal cancer ranks third in incidence and second in cancer-related deaths globally.
Major Risk Factors
- Genetic predisposition (e.g., Lynch syndrome, familial adenomatous polyposis)
- Chronic inflammatory conditions (e.g., Crohn’s disease, ulcerative colitis)
- Helicobacter pylori infection (gastric cancer)
- Hepatitis B and C viruses (hepatocellular carcinoma)
- Smoking, alcohol consumption, and diet high in red or processed meats
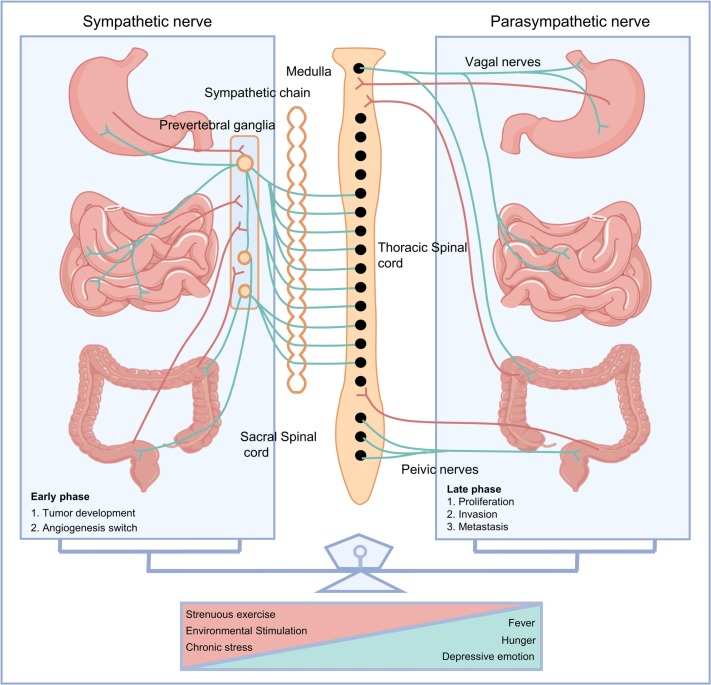
- Obesity and sedentary lifestyle
Classification of GI Tract Malignancies
Esophageal Cancer
Primarily squamous cell carcinoma or adenocarcinoma, often linked to tobacco, alcohol, and gastroesophageal reflux disease (GERD).
Gastric Cancer
Most commonly adenocarcinoma, often associated with H. pylori infection and dietary nitrosamines.
Small Intestine Tumors
Rare; typically neuroendocrine tumors, adenocarcinoma, or lymphoma.
Colorectal Cancer
One of the most common malignancies; risk increases with age, lifestyle, and family history.
Liver Cancer
Primarily hepatocellular carcinoma (HCC), often secondary to viral hepatitis or cirrhosis.
Pancreatic Cancer
Highly aggressive; primarily ductal adenocarcinoma, often diagnosed at advanced stages.
Clinical Presentation and Diagnostic Workup
Common Symptoms
- Unexplained weight loss
- Persistent abdominal pain or discomfort
- Change in bowel habits (e.g., diarrhea, constipation, blood in stool)
- Jaundice (in hepatobiliary cancers)
- Dysphagia (in esophageal cancer)
- Anemia or gastrointestinal bleeding
Diagnostic Modalities
- Endoscopy and colonoscopy with biopsy
- CT, MRI, and PET scans for staging
- Tumor markers (e.g., CEA for colon cancer, AFP for HCC)
- Histopathological evaluation for definitive diagnosis
Staging and Prognostic Indicators
TNM Classification
Cancer staging is universally determined using the TNM system:
- T: Size and extent of the primary tumor
- N: Lymph node involvement
- M: Distant metastasis
Prognostic Factors
- Tumor grade and histology
- Lymphovascular invasion
- Surgical margin status
- Response to therapy
- Patient’s performance status
Treatment Modalities for GI Tract Malignancies
Surgical Resection
The cornerstone of curative treatment for localized malignancies. Procedures vary by tumor location (e.g., colectomy, gastrectomy, Whipple procedure).
Chemotherapy
Used as adjuvant, neoadjuvant, or palliative therapy. Regimens depend on tumor type and genetic profile.
Radiation Therapy
Employed for esophageal, rectal, and pancreatic cancers, often in combination with chemotherapy.
Targeted and Immunotherapies
- HER2 inhibitors in gastric cancer
- EGFR and VEGF inhibitors in colorectal cancer
- Checkpoint inhibitors (e.g., PD-1 blockers) in MSI-high tumors
Palliative Care
Focused on symptom control and quality of life in advanced stages.
Preventive Strategies and Screening
Screening Recommendations
- Colorectal cancer: Colonoscopy starting at age 45–50
- Esophageal and gastric cancers: Screening in high-risk populations
- Liver cancer: Regular ultrasound and AFP levels in cirrhotic patients
Lifestyle Modifications
- High-fiber, low-fat diet rich in fruits and vegetables
- Smoking cessation and limiting alcohol intake
- Weight control and physical activity
Primary malignant neoplasms of the gastrointestinal tract encompass a range of complex and life-threatening cancers. Timely diagnosis through vigilant screening, personalized treatment strategies, and preventive health behaviors are essential to improving survival outcomes. Interdisciplinary collaboration among oncologists, gastroenterologists, surgeons, and radiologists remains pivotal in delivering optimal patient care.