Primary hypogonadism is a clinical condition characterized by impaired testicular function resulting in reduced testosterone production and/or impaired spermatogenesis. When this condition arises as a consequence of bilateral torsion of the testes, it becomes a urological and endocrinological emergency with long-term reproductive and hormonal implications.
In primary hypogonadism due to bilateral testicular torsion, the underlying issue lies within the testes themselves, leading to failure in hormone secretion and gamete production, independent of pituitary or hypothalamic dysfunction.
Bilateral Testicular Torsion: A Rare but Devastating Cause
What Is Testicular Torsion?
Testicular torsion refers to the twisting of the spermatic cord, which obstructs blood flow to the testicle. This condition is most commonly unilateral, affecting one testicle. However, bilateral torsion, where both testes are simultaneously involved, is rare and results in significant ischemia and testicular necrosis if not promptly addressed.
Mechanism of Injury
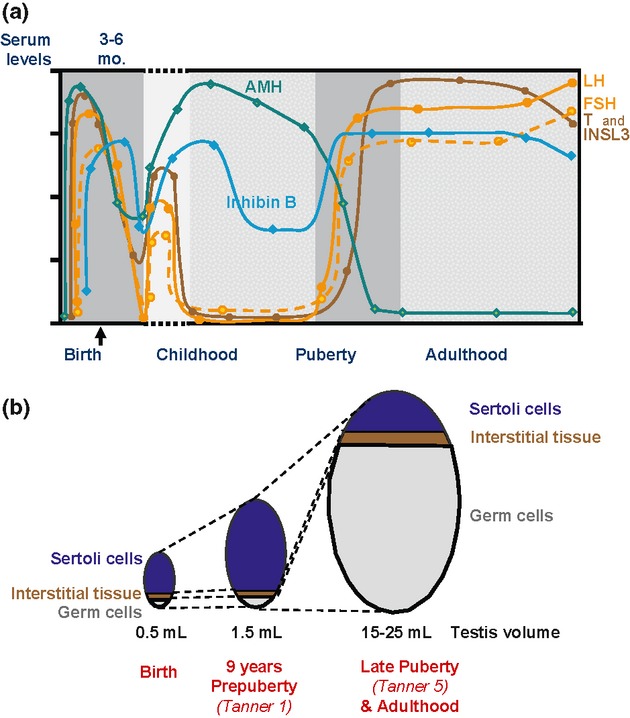
The ischemic injury from torsion leads to infarction of testicular tissue. In bilateral cases, complete loss of Leydig and Sertoli cell function can occur, resulting in irreversible testicular failure. Without functional testicular tissue, testosterone synthesis halts, and spermatogenesis ceases, leading to primary hypogonadism.
Clinical Presentation and Diagnostic Indicators
Symptoms and Initial Assessment
Patients with bilateral torsion typically present with:
- Acute, severe scrotal pain
- Swelling and erythema
- Nausea or vomiting
- Absence of cremasteric reflex bilaterally
Diagnostic Tools
- Scrotal Doppler Ultrasound: Reveals absent or diminished blood flow in both testes.
- Hormonal Panel:
- Elevated luteinizing hormone (LH)
- Elevated follicle-stimulating hormone (FSH)
- Decreased serum testosterone
- Semen analysis: Often shows azoospermia or severe oligospermia post-injury.
Pathophysiology of Hormonal Disruption
The disruption in Leydig cell function due to ischemic necrosis directly impairs testosterone synthesis. Simultaneously, Sertoli cell dysfunction eliminates spermatogenesis, triggering compensatory hypersecretion of gonadotropins from the pituitary—an endocrine hallmark of hypergonadotropic hypogonadism.
Management and Treatment Strategies
Emergency Surgical Intervention
Urgent scrotal exploration and bilateral detorsion are critical. Time is of the essence—testicular salvage is possible within 4–6 hours of symptom onset. In bilateral cases, orchiectomy may be necessary if necrosis is irreversible.
Hormonal Replacement Therapy
Patients who have lost testicular function require lifelong testosterone replacement therapy (TRT):
- Intramuscular injections (testosterone enanthate or cypionate)
- Transdermal patches or gels
- Subcutaneous testosterone pellets
Goals of TRT:
- Restore normal serum testosterone levels
- Preserve muscle mass, bone density, and libido
- Improve mood and energy
Fertility Preservation and Counseling
- Sperm banking before surgery is ideal, though often not feasible in acute torsion.
- Assisted reproductive techniques (ART) may be considered later if partial testicular function remains.
- Psychological counseling is essential for long-term quality of life.
Long-Term Outlook and Monitoring
Patients require lifelong monitoring of:
- Serum testosterone
- Hematocrit and hemoglobin (risk of polycythemia with TRT)
- Prostate-specific antigen (PSA) in aging males
- Bone mineral density
- Mood and cognitive function
Close collaboration between urologists, endocrinologists, and reproductive specialists is vital to optimizing outcomes.
Differential Diagnosis
Though bilateral testicular torsion is a clear-cut cause of primary hypogonadism, it is important to distinguish it from other etiologies:
- Klinefelter syndrome
- Cryptorchidism
- Mumps orchitis
- Testicular trauma
- Chemotherapy or radiation exposure
Each requires distinct diagnostic approaches and management strategies.
Preventive Considerations
- Early recognition of torsion signs is key to preventing testicular loss.
- Education campaigns targeting adolescent males and their caregivers can improve outcomes.
- Genital exams during routine pediatric and adolescent check-ups can help identify predisposing anatomical factors such as the bell-clapper deformity.
Primary hypogonadism resulting from bilateral testicular torsion is a rare but significant urological emergency that demands swift diagnosis and immediate surgical management. With timely intervention and appropriate hormonal replacement therapy, long-term outcomes can be managed effectively. Multidisciplinary care remains central to optimizing both physiological and psychological recovery in affected individuals.