Radiation therapy remains a cornerstone in the treatment of head and neck cancers, yet xerostomia—commonly known as dry mouth—is one of its most prevalent and debilitating side effects. Resulting from salivary gland hypofunction due to radiation exposure, xerostomia significantly impairs oral health, nutrition, speech, and quality of life. Preventing xerostomia secondary to radiation therapy requires a multifaceted clinical approach encompassing advanced radiotherapy techniques, pharmacologic agents, salivary substitutes, and patient-centered oral care.
Understanding Radiation-Induced Xerostomia: Mechanisms and Risk Factors
Pathophysiology of Salivary Gland Damage
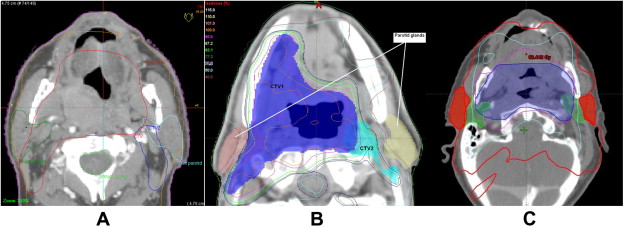
Ionizing radiation damages salivary acinar cells, endothelial cells, and ductal structures, leading to a reduction in salivary flow. Parotid, submandibular, and minor salivary glands are particularly vulnerable due to their radiosensitivity. The degree of xerostomia correlates with radiation dose, gland volume exposure, and fractionation schedule.
Key risk factors include:
- Radiation dose ≥ 26 Gy to the parotid glands
- Bilateral irradiation fields
- Older age and preexisting comorbidities
- Concurrent chemotherapy increasing toxicity
Advanced Radiotherapy Techniques for Salivary Gland Protection
Intensity-Modulated Radiation Therapy (IMRT)
IMRT has revolutionized xerostomia prevention by enabling precise dose distribution that spares salivary gland tissue. By conforming the radiation beam to the tumor’s shape, IMRT significantly reduces mean radiation doses to the parotid and submandibular glands without compromising tumor control.
Clinical outcomes:
- Reduced incidence of Grade 2–3 xerostomia
- Improved salivary flow rates at 12–24 months post-treatment
- Enhanced patient-reported quality of life
Proton Beam Therapy (PBT)
PBT offers further refinement in tissue-sparing capabilities due to the Bragg peak effect, which minimizes dose beyond the tumor target. Studies have shown reduced xerostomia rates when PBT is employed in select patients with favorable tumor anatomy.
Pharmacologic Approaches to Xerostomia Prevention
Amifostine: A Radioprotective Agent
Amifostine (Ethyol) is an FDA-approved cytoprotective drug administered intravenously before radiation. It scavenges free radicals and protects DNA in healthy tissues.
Efficacy highlights:
- Preserves salivary function by reducing parotid gland toxicity
- Decreases both acute and late-stage xerostomia
- Most beneficial when combined with IMRT
Limitations:
- Potential side effects include nausea, hypotension, and vomiting
- Requires administration under medical supervision
Pilocarpine and Cevimeline: Parasympathomimetic Sialogogues
These agents stimulate residual salivary gland tissue via muscarinic receptor activation.
- Pilocarpine: 5 mg orally three times daily
- Cevimeline: 30 mg orally three times daily
Usage Considerations:
- Indicated for patients with partial gland function
- May cause sweating, flushing, and gastrointestinal upset
Topical and Supportive Therapies
Artificial Saliva Substitutes and Oral Moisturizers
Non-pharmacologic interventions include:
- Salivary gels containing carboxymethylcellulose
- Mouth sprays with xylitol and fluoride
- Humidification devices for nighttime relief
Sugar-Free Chewing Gum and Lozenges
Stimulate saliva production via gustatory and masticatory pathways. Xylitol-based options also help in dental caries prevention.
Nutritional and Oral Care Strategies
Hydration and Diet
- Encourage regular water intake throughout the day
- Avoid caffeine, alcohol, and acidic or spicy foods
- Emphasize moist, soft-textured meals and adequate protein
Oral Hygiene Practices
- Use fluoride toothpaste and alcohol-free mouth rinses
- Brush with ultra-soft bristles to prevent mucosal trauma
- Regular dental visits to monitor for caries and fungal infections
Novel and Emerging Therapies
Gene Therapy and Regenerative Approaches
- Aquaporin-1 gene therapy shows promise in restoring salivary flow via adenoviral vectors
- Stem cell therapy aims to regenerate damaged glandular tissues
Low-Level Laser Therapy (LLLT)
- Enhances tissue repair and stimulates salivary gland activity
- Non-invasive adjunct therapy with minimal adverse effects
Patient-Centered Xerostomia Management Plans
Multidisciplinary Care Coordination
- Radiation oncologists, dentists, dietitians, and speech therapists must collaborate pre-treatment and throughout care
- Salivary gland function assessments (sialometry, scintigraphy) help track progression
Patient Education and Symptom Tracking
- Educate patients on early signs of xerostomia
- Use patient-reported outcome measures (e.g., Xerostomia Questionnaire, EORTC QLQ-H&N35)
The prevention of xerostomia secondary to radiation therapy necessitates an integrated approach rooted in technological advancement, clinical pharmacology, supportive care, and patient empowerment. By prioritizing salivary gland preservation through IMRT or PBT, leveraging protective agents like amifostine, and ensuring consistent oral care, we can significantly reduce the burden of xerostomia. Coordinated multidisciplinary efforts are essential to safeguard the quality of life in patients undergoing head and neck cancer treatment.

