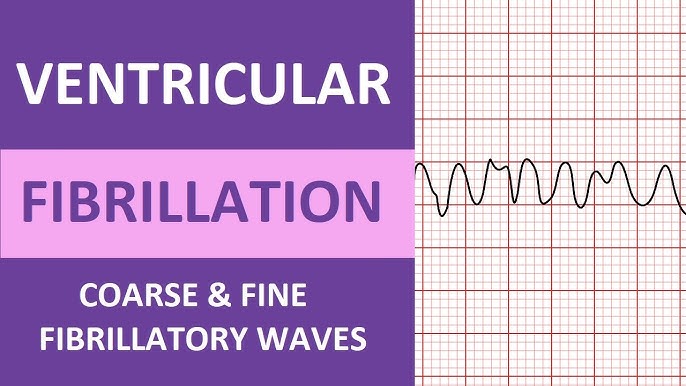
Ventricular fibrillation (VF) is a life-threatening arrhythmia characterized by chaotic, ineffective electrical activity in the ventricles, resulting in cessation of effective cardiac output and sudden cardiac arrest. Immediate intervention is critical, but long-term prevention is essential for at-risk populations. This article provides a structured, evidence-based approach to the prevention of ventricular fibrillation, emphasizing risk stratification, pharmacologic and device-based therapies, lifestyle modification, and advanced cardiac care.
Understanding the Pathophysiology of Ventricular Fibrillation
Ventricular fibrillation arises when the ventricular myocardium exhibits disorganized electrical impulses, leading to rapid, uncoordinated contractions. The primary mechanisms include:
- Reentrant circuits due to myocardial scar or ischemia
- Triggered activity from early or delayed afterdepolarizations
- Automaticity abnormalities in Purkinje fibers or other cardiac cells
VF is commonly the final event in ischemic heart disease, cardiomyopathies, and inherited arrhythmia syndromes.
Risk Stratification for Ventricular Fibrillation
High-Risk Populations
- History of myocardial infarction or ischemic cardiomyopathy
- Ejection fraction (EF) ≤ 35%
- Prior episode of ventricular tachycardia or fibrillation
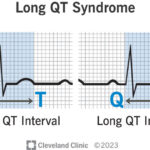
- Genetic conditions such as Brugada syndrome, long QT syndrome, or catecholaminergic polymorphic ventricular tachycardia (CPVT)
Diagnostic Tools
- Electrocardiogram (ECG): Identification of arrhythmogenic patterns
- Echocardiography: Evaluation of EF and structural abnormalities
- Holter Monitoring: Detection of premature ventricular contractions (PVCs) and non-sustained VT
- Electrophysiological Study (EPS): Assessment of inducibility of ventricular arrhythmias
Pharmacologic Approaches to Prevent Ventricular Fibrillation
Beta-Blockers
Beta-adrenergic blockers reduce sympathetic stimulation, a known trigger for VF. They are particularly effective post-myocardial infarction and in inherited arrhythmia syndromes.
Common options:
- Metoprolol succinate
- Bisoprolol
- Carvedilol
Antiarrhythmic Medications
- Amiodarone: Effective for both ischemic and non-ischemic cardiomyopathy
- Sotalol: Used cautiously due to proarrhythmic risks
- Lidocaine or mexiletine: Considered in acute ischemia-related VF
Note: Antiarrhythmic therapy should be tailored to patient-specific comorbidities and continuously monitored for QT prolongation and torsadogenic potential.
Implantable Cardioverter-Defibrillators (ICDs): Gold Standard in VF Prevention
Primary Prevention
Indicated for patients with:
- LVEF ≤ 35% due to prior myocardial infarction or cardiomyopathy
- NYHA Class II or III heart failure symptoms
Secondary Prevention
ICD placement is essential for survivors of cardiac arrest or documented VF not due to reversible causes.
Advantages:
- Automatic detection and termination of VF
- Long-term survival benefit demonstrated in randomized trials (e.g., MADIT-II, SCD-HeFT)
Catheter Ablation for VF Substrate Modification
For patients with recurrent VF episodes or frequent ICD shocks, catheter ablation may be considered:
- Targets the arrhythmogenic substrate, often scar tissue in the left ventricle
- Reduces PVC burden and electrical storm episodes
- Enhances ICD performance by reducing therapy delivery
This approach is most effective when guided by electroanatomic mapping and in combination with imaging modalities such as cardiac MRI.
Lifestyle and Comorbidity Management
Cardiac Rehabilitation and Exercise
- Structured rehabilitation programs reduce sympathetic tone and improve cardiac function
- Avoidance of excessive exertion in patients with channelopathies or structural heart disease
Control of Modifiable Risk Factors
- Hypertension, diabetes, dyslipidemia, and smoking should be aggressively managed
- Weight reduction and sleep apnea treatment can improve cardiac electrophysiology and decrease arrhythmic risk
Prevention in Inherited Arrhythmia Syndromes
Patients with inherited arrhythmogenic disorders require tailored interventions:
Long QT Syndrome (LQTS)
- Beta-blockers
- ICDs for high-risk patients
- Avoid QT-prolonging drugs
Brugada Syndrome
- ICDs in symptomatic or high-risk patients
- Quinidine may be used to suppress VF episodes
Catecholaminergic Polymorphic VT (CPVT)
- Beta-blockers and flecainide
- ICDs with caution due to potential proarrhythmia
Emergency Preparedness and Community Measures
- Automated External Defibrillators (AEDs) should be available in public spaces
- Bystander CPR training enhances survival from sudden cardiac arrest
- Patient education on recognizing prodromal symptoms such as palpitations, syncope, or chest discomfort
Current Guidelines and Consensus Recommendations
ACC/AHA/HRS Guidelines
- Strong recommendation for ICDs in patients with prior VF or LVEF ≤ 35%
- Routine use of beta-blockers post-MI
- Selective use of amiodarone or sotalol for arrhythmia suppression
ESC Guidelines
- Emphasis on genetic testing in inherited arrhythmias
- Support for ablation in refractory cases
- Promotion of multidisciplinary care including cardiologists, electrophysiologists, and genetic counselors
The prevention of ventricular fibrillation requires a multifaceted approach encompassing risk stratification, pharmacologic therapy, device implantation, and lifestyle modification. Implantable cardioverter-defibrillators remain the most effective tool in both primary and secondary prevention. As the understanding of electrophysiological and genetic contributors to VF deepens, personalized strategies continue to evolve, offering improved outcomes for patients at risk of sudden cardiac death.