Glanzmann’s thrombasthenia (GT) is a rare inherited bleeding disorder caused by defects in the platelet glycoprotein IIb/IIIa complex, which is essential for platelet aggregation. As a result, individuals with GT experience impaired platelet function, leading to increased susceptibility to bleeding, especially during and after surgical procedures. Surgical interventions in patients with GT require careful planning and tailored hemostatic strategies to minimize the risk of bleeding complications.
Pathophysiology of Glanzmann’s Thrombasthenia
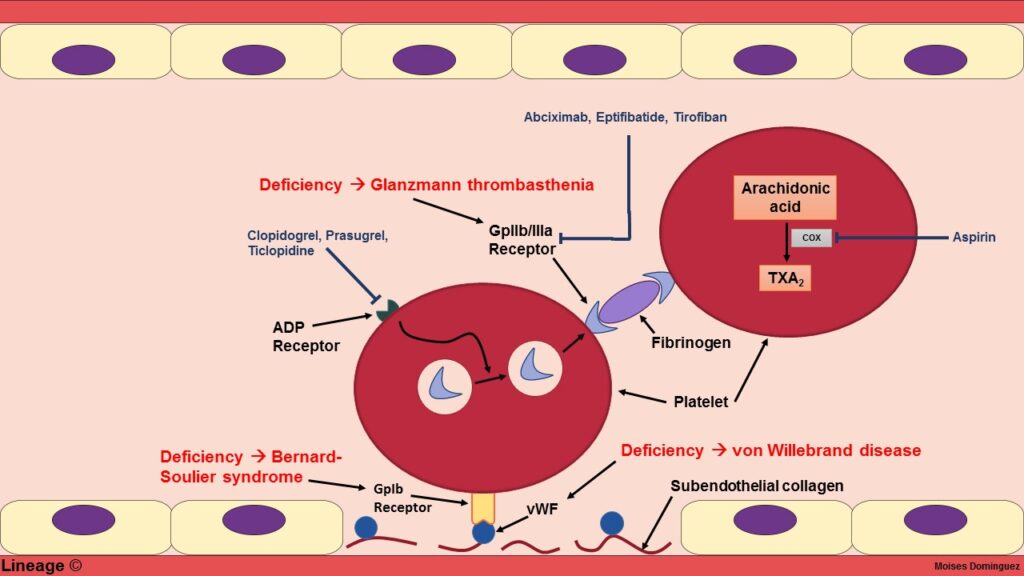
In Glanzmann’s thrombasthenia, the deficiency or dysfunction of the integrin αIIbβ3 (the platelet fibrinogen receptor) results in defective platelet aggregation. This defect significantly impairs the ability of platelets to form stable clots, even in the presence of normal platelet counts. Given this impaired platelet aggregation, individuals with GT face substantial challenges during any surgical or invasive procedure.
Understanding the pathophysiology is key to developing a targeted approach for preventing surgery-induced bleeding in patients with Glanzmann’s thrombasthenia.
Preoperative Planning for Glanzmann’s Thrombasthenia
Detailed Patient History and Assessment
Before any surgery, a thorough preoperative evaluation is critical. Key aspects include:
- Medical History: Review the patient’s history of spontaneous bleeding episodes, surgical history, and any previous responses to bleeding management.
- Platelet Function Testing: Specialized tests, including platelet aggregation studies, should be conducted to confirm the diagnosis and assess the severity of platelet dysfunction.
- Coagulation Profiles: Ensure there is no coexisting coagulation disorder by evaluating prothrombin time (PT), activated partial thromboplastin time (aPTT), and fibrinogen levels.
Evaluation of Surgical Procedure
The type of surgery plays a significant role in determining the risk of bleeding. Surgeries with higher risks of bleeding, such as major surgeries (e.g., abdominal or cardiac procedures), require more intensive management. For minor procedures, such as dental extractions, desmopressin or antifibrinolytics may be sufficient.
Hemostatic Therapy in Glanzmann’s Thrombasthenia: Key Strategies
Platelet Transfusion Therapy
Platelet transfusions are the cornerstone of hemostatic therapy for Glanzmann’s thrombasthenia. The primary goal is to increase the number of functionally active platelets in circulation. The following platelet transfusion strategies are used:
- Platelet Transfusion Preoperatively:
For major surgeries, patients should receive platelet transfusions 1-2 hours before the procedure to ensure adequate platelet function. The transfusion dose is typically 1-2 units of platelets per 10 kg of body weight. - Continuous Platelet Support:
During major surgeries, the patient may require additional platelet transfusions every 24-48 hours, depending on ongoing bleeding and platelet count. - Platelet Crossmatching:
Platelet crossmatching may be needed to ensure that transfused platelets are compatible with the patient’s antibodies.
Recombinant Activated Factor VII (rFVIIa)
In some cases where platelet transfusion alone is insufficient or where the surgery involves high bleeding risks, recombinant activated factor VII (rFVIIa) may be administered to promote clot formation. rFVIIa is particularly useful in the perioperative setting to augment hemostasis, especially when there is significant platelet dysfunction.
- Administration:
rFVIIa is given intravenously and is often used in conjunction with platelet transfusions for enhanced efficacy. - Indications:
This therapy is especially valuable in cases of severe bleeding or complex surgeries, such as neurosurgical or cardiac procedures.
Antifibrinolytic Agents in Surgery for Glanzmann’s Thrombasthenia
Role of Antifibrinolytics
Antifibrinolytics such as tranexamic acid or aminocaproic acid are often used as adjunctive therapy in surgeries with a moderate to high risk of bleeding. These agents work by inhibiting the breakdown of fibrin, thereby stabilizing the clot and reducing bleeding.
- Indications:
These medications are particularly useful in surgeries where mucosal bleeding is expected, such as dental procedures, tonsillectomies, or ENT surgeries. - Dosage and Administration:
- Tranexamic acid: Typically administered intravenously or orally, depending on the surgical procedure.
- Aminocaproic acid: Also used intravenously during major procedures to control bleeding.
Combination Therapy for Optimal Results
In many cases, a combination of platelet transfusion, rFVIIa, and antifibrinolytic agents may be necessary, particularly in complex or high-risk surgeries. The exact regimen depends on individual patient factors, including the severity of GT, the type of surgery, and the patient’s response to treatment.
Surgical Procedure Categories and Tailored Hemostatic Approaches
The type of surgery significantly influences the choice of hemostatic therapy. Procedures can generally be categorized as follows:
| Surgical Type | Bleeding Risk | Recommended Approach |
|---|---|---|
| Minor (e.g., dental extractions) | Low | Platelet transfusion + antifibrinolytics |
| Moderate (e.g., tonsillectomy) | Moderate | Platelet transfusion + tranexamic acid |
| Major (e.g., abdominal, cardiac) | High | Platelet transfusion + rFVIIa + antifibrinolytics |
| Neurosurgical or Cardiac | Very High | Platelet transfusion + rFVIIa + close monitoring |
For high-risk surgeries, more aggressive monitoring and adjustment of platelet transfusions are necessary to ensure hemostatic stability throughout the procedure.
Postoperative Monitoring and Management
After surgery, continuous monitoring is critical to detect and manage bleeding complications. Key areas of focus include:
- Platelet Count and Function:
Ongoing platelet transfusions may be necessary if counts fall below the therapeutic threshold. The functionality of platelets should also be assessed postoperatively. - Signs of Bleeding:
Wound inspections, imaging studies (if applicable), and observation for any signs of internal bleeding or bruising should be conducted routinely. - Hemoglobin and Hematocrit Levels:
Regular checks of hemoglobin and hematocrit are important to detect any ongoing blood loss.
Preventing surgery-induced bleeding in Glanzmann’s thrombasthenia requires a multifaceted approach that incorporates platelet transfusion, adjunctive therapies, and vigilant postoperative care. By tailoring hemostatic strategies to the individual patient and the specific surgical procedure, clinicians can significantly reduce bleeding complications. The optimal management strategy involves preoperative preparation, real-time monitoring, and personalized care to ensure the best possible surgical outcomes for patients with Glanzmann’s thrombasthenia.