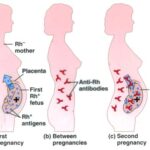
Rh isoimmunization, or Rh sensitization, occurs when an Rh-negative woman is exposed to Rh-positive fetal red blood cells (RBCs), leading to the production of anti-D antibodies. In future pregnancies, these antibodies may cross the placenta and attack Rh-positive fetal cells, resulting in hemolytic disease of the fetus and newborn (HDFN).
Even minimal fetomaternal hemorrhage during first-trimester pregnancy termination, whether spontaneous (miscarriage) or induced (surgical or medical abortion), can result in Rh sensitization. Therefore, preventive protocols must be strictly observed regardless of gestational age.
Mechanism of Rh Sensitization in Early Gestation
Fetal-maternal hemorrhage (FMH) can occur as early as 6–8 weeks of gestation. During pregnancy termination, the disruption of chorionic villi and trophoblasts can cause fetal RBCs to enter the maternal circulation. If the mother is Rh-negative and the fetus is Rh-positive, her immune system may recognize the D antigen as foreign, initiating an alloimmune response.
This immune response develops silently, making preventive intervention crucial during the first exposure to avoid irreversible sensitization.
Indications for Rh Immunoglobulin After First-Trimester Pregnancy Termination
The American College of Obstetricians and Gynecologists (ACOG), Royal College of Obstetricians and Gynaecologists (RCOG), and other major bodies recommend anti-D immunoglobulin prophylaxis in the following situations involving Rh-negative women:
- Surgical abortion (dilation and curettage or vacuum aspiration)
- Medical abortion using mifepristone and misoprostol
- Spontaneous abortion (miscarriage), including incomplete or threatened miscarriage
- Molar pregnancy or ectopic pregnancy
- Manual uterine evacuation for retained products
The goal is to administer anti-D immunoglobulin promptly and prevent maternal sensitization to Rh-positive fetal RBCs.
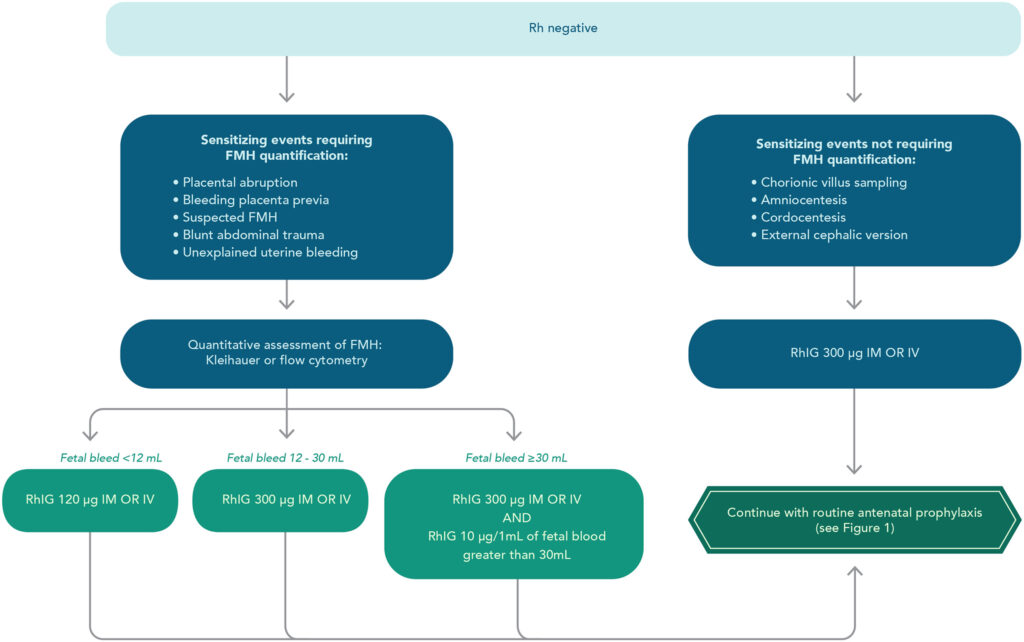
Recommended Dosage and Administration of Anti-D Immunoglobulin
Standard Protocol
- Dose: 50 µg IM (covers up to 2.5 mL of fetal RBCs) or 100–120 IU for pregnancies under 12 weeks
- Timing: Within 72 hours of the termination event
- If there is uncertainty about fetal Rh status, prophylaxis is still advised to err on the side of caution.
In cases where prophylaxis was not administered within 72 hours, it may still be given up to 13 days post-event to offer partial protection.
Testing and Confirmation: Maternal and Fetal Rh Status
In early pregnancy, fetal Rh typing is rarely performed due to limited fetal blood presence. Thus, the standard approach is to:
- Determine maternal Rh status via blood typing
- If the woman is Rh-negative, administer RhIg unless fetal Rh is confirmed negative, which is seldom practical in early termination
This simplifies clinical decision-making and maximizes the protective scope.
Clinical Guidelines for Medical vs. Surgical Termination
Medical Termination
- Medications such as mifepristone and misoprostol induce uterine contractions, increasing FMH risk.
- Anti-D prophylaxis is recommended for all Rh-negative women, even if the abortion is completed at home or in outpatient settings.
Surgical Termination
- Greater risk of FMH due to mechanical disruption of the uterus and gestational sac.
- Mandatory anti-D administration for Rh-negative patients undergoing dilation and curettage or suction evacuation.
Consequences of Failing to Prevent Rh Isoimmunization
Without prophylaxis, the risk of Rh sensitization after first-trimester abortion ranges from 1.5% to 2%, depending on the procedure and fetal Rh status. The long-term implications include:
- Hemolytic disease of future Rh-positive fetuses
- Need for intrauterine transfusions
- Neonatal jaundice, anemia, and kernicterus
- Compromised reproductive health and pregnancy outcomes
Prevention is significantly more effective, safer, and cost-efficient than managing Rh disease after sensitization occurs.
Institutional Policy Recommendations
To ensure universal protection against Rh sensitization:
- Mandatory Rh typing for all early pregnancy losses and terminations
- Routine stocking of low-dose RhIg (50 µg) in abortion and emergency care clinics
- Standardized protocols for administration timing and documentation
- Training healthcare providers on the necessity of RhIg even in early gestation
By establishing such measures, healthcare systems can eliminate preventable cases of Rh alloimmunization.
Ethical Considerations in Prophylaxis
All Rh-negative women should be counseled about:
- The importance of anti-D immunoglobulin post-termination
- The potential effects of future sensitization if prophylaxis is not administered
- Their right to decline RhIg, although strongly discouraged
Informed consent and shared decision-making are essential, particularly when prophylaxis is offered prophylactically due to uncertainty in fetal Rh status.
Preventing Rh isoimmunization at the time of first-trimester pregnancy termination is a vital component of reproductive health care for Rh-negative women. Administering anti-D immunoglobulin promptly and consistently, even when fetal Rh status is unknown, eliminates the risk of maternal sensitization and protects future pregnancies from severe complications. Universal adherence to this practice represents the highest standard of preventive medicine in obstetric care.