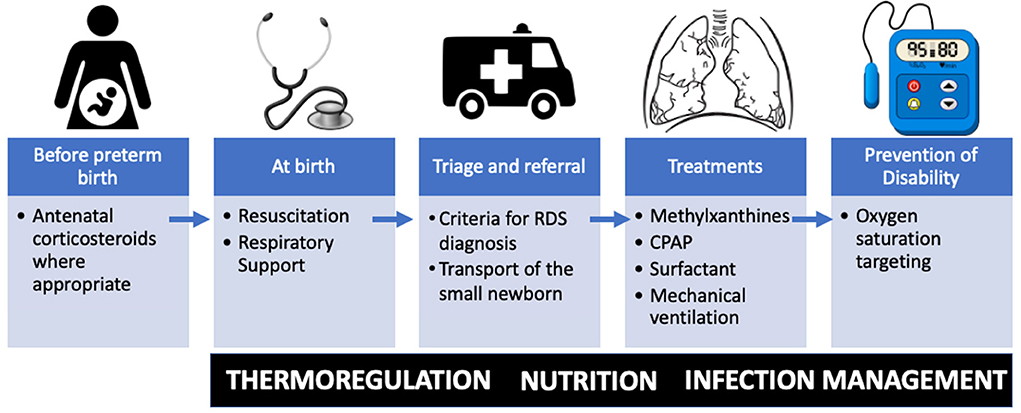
Respiratory Distress Syndrome (RDS) in newborns is a critical condition primarily caused by insufficient production of pulmonary surfactant, most commonly affecting preterm infants. Surfactant is essential for reducing surface tension in the alveoli, preventing collapse during expiration. Without timely intervention, RDS can lead to significant morbidity and mortality. Preventive strategies must be initiated during the antenatal period, continue through labor, and extend into the immediate postnatal phase to ensure the best outcomes for at-risk neonates.
Etiology and Risk Factors of RDS in Newborns
Understanding the underlying causes of neonatal RDS allows for targeted preventive efforts.
Major Risk Factors
- Premature birth (<34 weeks gestation)
- Cesarean delivery without labor
- Male sex
- Perinatal asphyxia
- Maternal diabetes mellitus
- Second-born twin or higher-order multiples
- Genetic predisposition or surfactant protein deficiency
Antenatal Interventions to Prevent RDS
Administration of Antenatal Corticosteroids
Antenatal corticosteroids are the cornerstone of RDS prevention in preterm births between 24–34 weeks gestation.
- Recommended agents: Betamethasone or dexamethasone
- Mechanism: Accelerates fetal lung maturation and surfactant production
- Dosage protocol: Two doses of betamethasone 12 mg IM 24 hours apart, or four doses of dexamethasone 6 mg every 12 hours
- Outcomes: Reduces incidence of RDS by up to 50%, decreases need for mechanical ventilation, and lowers neonatal mortality
Tocolysis for Delaying Preterm Delivery
Short-term tocolytic therapy (e.g., nifedipine, atosiban) may delay preterm labor, providing a window for corticosteroid administration and in-utero transfer to a tertiary facility.
Management of Maternal Conditions
- Optimal glycemic control in diabetic mothers enhances fetal lung maturity.
- Infection screening and treatment (e.g., Group B Streptococcus, chorioamnionitis) minimize systemic inflammatory impacts on fetal lungs.
Perinatal Strategies to Reduce RDS Risk
Timing and Mode of Delivery
- Avoid elective cesarean delivery before 39 weeks unless medically indicated.
- Vaginal delivery or induction of labor allows for stress-induced catecholamine surge, enhancing surfactant release and fluid clearance from neonatal lungs.
Intrapartum Care
- Continuous fetal monitoring to detect distress
- Delayed cord clamping to promote improved cardiovascular stability and transition to postnatal respiration
- Neonatal resuscitation preparedness for high-risk deliveries
Immediate Postnatal Interventions
Early CPAP (Continuous Positive Airway Pressure)
For spontaneously breathing preterm infants, early CPAP (within minutes of birth) is preferable to intubation:
- Prevents alveolar collapse
- Stimulates endogenous surfactant release
- Reduces the need for mechanical ventilation
Prophylactic vs Early Rescue Surfactant Therapy
Surfactant replacement therapy remains a key intervention in preventing and managing RDS.
- Prophylactic surfactant: Administered within 15 minutes of birth in extremely preterm infants (<26 weeks)
- Early rescue surfactant: Given to symptomatic infants with signs of RDS and increasing oxygen requirements
- Preferred agents include poractant alfa or beractant
Less Invasive Surfactant Administration (LISA)
- A catheter-based method for delivering surfactant while avoiding intubation
- Associated with reduced incidence of bronchopulmonary dysplasia and ventilation-associated complications
Supportive Care and Long-Term Respiratory Management
Thermal Regulation and Fluid Balance
- Maintain normothermia to prevent increased metabolic demands
- Monitor and manage fluid intake to reduce risk of pulmonary edema
Nutritional Support
- Early initiation of parenteral nutrition and advancement to enteral feeding
- Promotes overall growth and lung development
Caffeine Therapy
- Used for apnea of prematurity, but also shown to reduce BPD and duration of mechanical ventilation
Clinical Evidence Supporting Prevention of RDS
- NICHD trials have demonstrated the significant efficacy of corticosteroids in reducing RDS and neonatal mortality.
- COIN and SUPPORT trials endorse early CPAP as a safer alternative to immediate intubation in preterm neonates.
- Meta-analyses confirm that prophylactic surfactant, particularly via LISA, results in better respiratory outcomes.
Innovations and Future Directions
Stem Cell Therapies
Research into mesenchymal stem cells (MSCs) suggests potential in modulating lung inflammation and promoting repair in preterm infants at risk of RDS.
Artificial Surfactants
Next-generation synthetic surfactants are being developed with improved efficacy and fewer immunologic reactions.
Personalized Neonatal Care
- Genetic profiling to identify infants at highest RDS risk
- Biomarker-based screening for tailored corticosteroid dosing
Preventing respiratory distress syndrome in the newborn necessitates a multifaceted and proactive approach, beginning with antenatal corticosteroids and continuing through delivery and postnatal care. By integrating pharmacologic, mechanical, and supportive strategies, we can significantly lower the incidence of RDS and improve neonatal respiratory outcomes, particularly among preterm infants. Ongoing innovations in respiratory support and personalized medicine hold promise for further advancements in neonatal care.