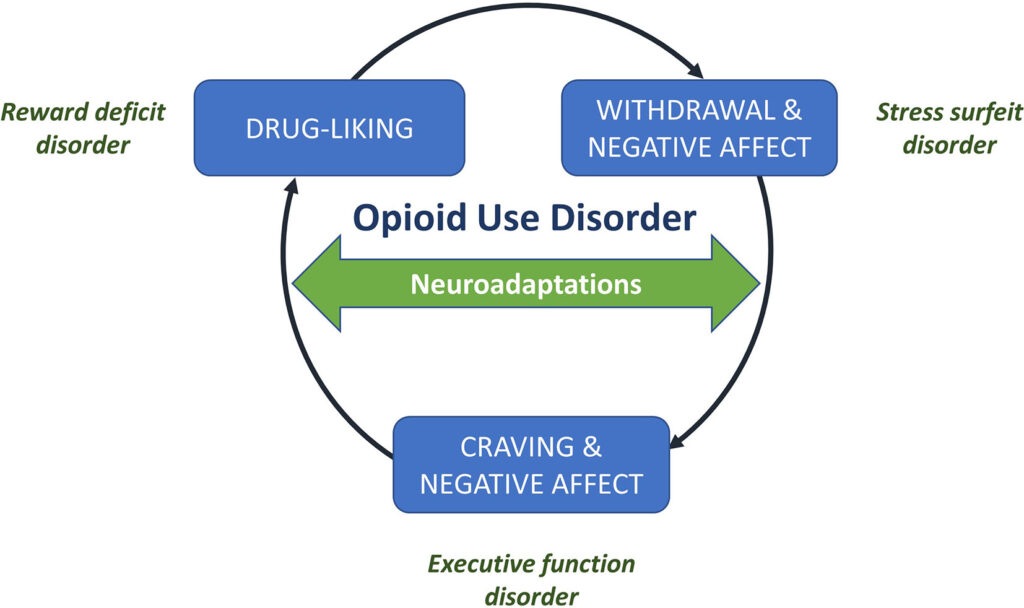
Opioid dependence is a chronic and relapsing condition characterized by compulsive opioid use despite harmful consequences. Even after successful detoxification, individuals with opioid use disorder (OUD) remain at high risk for relapse, particularly during the early stages of recovery. Effective relapse prevention is therefore essential to achieving long-term abstinence and improved quality of life.
The likelihood of relapse is influenced by a range of biological, psychological, and social factors. Addressing these through integrated, evidence-based interventions can significantly reduce recurrence and promote sustained recovery.
Key Risk Factors for Opioid Relapse
Understanding the triggers and vulnerabilities that contribute to relapse enables targeted prevention strategies.
Biological Factors
- Neuroadaptations in brain reward circuits
- Protracted withdrawal symptoms such as anxiety, insomnia, or dysphoria
- Co-occurring mental health disorders (e.g., depression, PTSD)
Psychological Triggers
- Cravings and intrusive thoughts
- Maladaptive coping mechanisms
- Low motivation or ambivalence toward recovery
Environmental and Social Influences
- Exposure to high-risk environments or people associated with past use
- Lack of support from family or community
- Socioeconomic stressors such as unemployment or housing instability
Medication-Assisted Treatment (MAT): The Foundation of Relapse Prevention
Methadone
- Full opioid agonist, administered under controlled clinical supervision
- Suppresses cravings and withdrawal
- Reduces mortality and criminal behavior
Buprenorphine
- Partial opioid agonist with ceiling effect, lowering overdose risk
- Often combined with naloxone to deter misuse (Suboxone®)
- Allows for office-based treatment and greater flexibility
Naltrexone
- Opioid antagonist that blocks euphoric effects of opioids
- Extended-release injectable formulation (Vivitrol®) ensures compliance
- Requires full detoxification prior to initiation
Benefits of MAT include improved treatment retention, reduced opioid use, lower risk of overdose, and enhanced psychosocial functioning.
Behavioral Therapies for Sustained Abstinence
Cognitive Behavioral Therapy (CBT)
- Helps patients identify and change distorted thinking patterns
- Teaches coping strategies to handle cravings and stress
- Enhances self-efficacy and relapse prevention skills
Contingency Management (CM)
- Provides tangible rewards for drug-free urine tests or treatment adherence
- Encourages positive reinforcement and accountability
Motivational Interviewing (MI)
- Strengthens personal motivation for change
- Addresses ambivalence in early recovery
12-Step Facilitation
- Introduces patients to mutual-help groups such as Narcotics Anonymous (NA)
- Emphasizes peer support and spiritual growth
Group and Family Therapy
- Builds communal support networks
- Involves family in recovery planning to repair relationships and prevent isolation
Holistic and Supportive Interventions
Psychoeducation
- Provides information on addiction, relapse triggers, and recovery pathways
- Empowers individuals to make informed choices about their care
Vocational Training and Employment Support
- Increases economic independence and reduces relapse linked to unemployment
Housing Stability and Sober Living Environments
- Safe and substance-free housing reduces exposure to relapse triggers
- Transitional living homes offer structure during early recovery
Physical Health and Wellness
- Exercise, nutrition, and sleep hygiene promote neurological healing
- Yoga, mindfulness, and meditation reduce stress and improve emotional regulation
Structured Relapse Prevention Plan
A personalized relapse prevention plan should include the following:
- Identification of triggers
- Development of coping skills
- Crisis management protocol
- Access to emergency contact network
- Regular follow-up appointments with care team
- Adherence to MAT and therapy schedule
Monitoring, Support, and Long-Term Care
Regular Urine Drug Screening
- Provides objective evidence of sobriety
- Helps identify early signs of relapse
Peer Support and Recovery Coaching
- Offers guidance from individuals with lived experience
- Reinforces commitment to abstinence
Long-Term Case Management
- Coordinates care across medical, psychiatric, and social domains
- Ensures continuity and addresses emerging needs
Technological Aids in Relapse Prevention
- Mobile apps offering daily check-ins, reminders, and coping tools
- Telemedicine for remote therapy sessions and MAT consultations
- Digital recovery communities that foster round-the-clock peer support
Key Indicators of Recovery Stability
- Adherence to medication and therapy
- Stable living and employment conditions
- Strong family and social support
- Improved physical and mental health
- Absence of cravings and high-risk behaviors
Future Directions in Relapse Prevention
- Personalized medicine using genetic markers to predict relapse risk
- Neurofeedback and brain stimulation therapies to repair neural pathways
- AI-powered predictive tools for early relapse detection
- Integration of trauma-informed care into all treatment modalities
The prevention of relapse to opioid dependence requires a comprehensive, sustained, and individualized approach that integrates pharmacological, behavioral, and psychosocial interventions. Long-term success depends on continuous monitoring, community engagement, and holistic support systems. With structured care and unwavering support, recovery from opioid dependence is both achievable and sustainable.