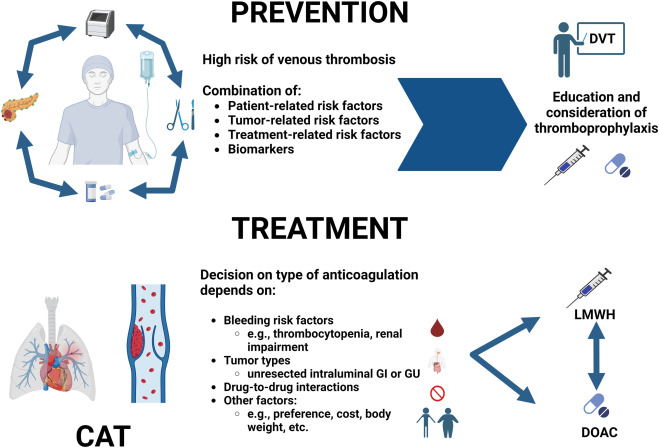
Venous thromboembolism (VTE), encompassing deep vein thrombosis (DVT) and pulmonary embolism (PE), is a frequent complication in patients with cancer. Known as cancer-associated thrombosis (CAT), this condition not only increases morbidity and mortality but also complicates oncological treatment. The prevention of recurrent venous thrombosis in malignancy is a clinical priority, as recurrence rates remain high despite anticoagulation, particularly in patients with active malignancy.
Pathophysiological Basis of Recurrent Thrombosis in Malignancy
Malignancy induces a prothrombotic state through multiple mechanisms:
- Tumor cell activation of coagulation cascade
- Expression of tissue factor and cancer procoagulant
- Endothelial dysfunction and platelet activation
- Chemotherapy and anti-angiogenic therapy impact
- Immobility and central venous catheters
This persistent hypercoagulable milieu sustains the risk of recurrent events even during anticoagulant therapy, necessitating tailored prevention strategies.
Risk Stratification for Recurrent Venous Thrombosis in Cancer
An accurate assessment of recurrence risk is essential to guide preventive therapy.
High-Risk Factors
- Active or metastatic cancer (especially pancreatic, gastric, brain, and lung)
- Ongoing chemotherapy or anti-angiogenic agents
- Previous VTE within 6 months
- Elevated D-dimer or platelet count
- Obesity and immobility
- Central venous catheter use
Clinical Tools
- Khorana Score (predicts initial VTE risk but less reliable for recurrence)
- Vienna CAT risk model
- COMPASS-CAT score for recurrence risk during treatment
Primary Approach: Long-Term Anticoagulation
Low Molecular Weight Heparin (LMWH)
LMWH has been the standard of care for prevention of recurrent CAT:
- Dalteparin, Enoxaparin, and Tinzaparin are commonly used
- Administered subcutaneously for a minimum of 6 months
- Superior to vitamin K antagonists (VKA) in reducing recurrence without increasing major bleeding
CLOT trial results support the extended use of LMWH beyond 6 months in selected patients with persistent cancer.
Direct Oral Anticoagulants (DOACs)
DOACs have emerged as oral alternatives with favorable efficacy profiles:
| DOAC | Key Findings |
|---|---|
| Edoxaban | Similar recurrence prevention to LMWH but higher bleeding risk in GI malignancies |
| Rivaroxaban | Effective in VTE prevention, caution with upper GI cancers |
| Apixaban | Lower bleeding risk, preferred in patients with high GI bleeding risk |
Duration typically ranges from 6 months to indefinite, based on cancer status and recurrence risk.
Duration of Anticoagulation: Individualized Based on Malignancy
- Active cancer or ongoing treatment: Continue anticoagulation indefinitely
- Complete remission and no thrombotic risk factors: Consider stopping after 6–12 months
- Frequent reassessment is necessary, especially in dynamic clinical scenarios
Special Considerations in Recurrence Prevention
Central Venous Catheter-Associated Thrombosis
- LMWH preferred for initial treatment
- Catheter removal may be necessary in non-essential use
- No prophylactic anticoagulation unless additional VTE risk factors are present
Thrombocytopenia Management
- In cases of low platelet counts (<50,000/µL), adjust anticoagulation:
- Hold or reduce dose in severe thrombocytopenia
- Use platelet transfusions to maintain safe levels for anticoagulation
Surgical and Procedural Considerations
- Temporary interruption may be needed for invasive procedures
- Bridging strategies must consider thrombosis vs bleeding risk
Adjunctive Measures for Recurrence Prevention
Mechanical Prophylaxis
- Graduated compression stockings and intermittent pneumatic compression in hospitalized or immobile patients
Early Ambulation
- Strongly encouraged postoperatively and in hospital stays to reduce stasis
Lifestyle and Supportive Measures
- Hydration, physical activity, and addressing modifiable risk factors
- Nutritional support and control of comorbidities
Monitoring and Follow-Up Strategy
Regular Laboratory Monitoring
- D-dimer trends may predict recurrence
- CBC for thrombocytopenia and anemia
- Renal function for dose adjustments
Imaging Surveillance
- Not routinely recommended unless clinical suspicion of recurrence
- Consider Doppler ultrasound or CT pulmonary angiography if symptoms arise
Future Directions in Cancer-Associated Thrombosis Management
- Tailored therapy based on tumor type, genetics, and thrombosis biomarkers
- Extended DOAC indications with safety data for high-bleeding-risk malignancies
- Real-world data registries to improve recurrence prediction and personalize therapy
- Development of risk calculators integrating genomic and proteomic markers
Preventing recurrent venous thrombosis in malignancy requires an integrated, patient-specific approach grounded in evidence-based anticoagulation, vigilant monitoring, and dynamic reassessment. With the evolving landscape of oncology and thrombosis management, clinicians must remain informed and agile in applying the latest therapeutic strategies. Early intervention, long-term anticoagulation when indicated, and individualized follow-up protocols significantly reduce the burden of recurrence and improve overall outcomes in this vulnerable population.