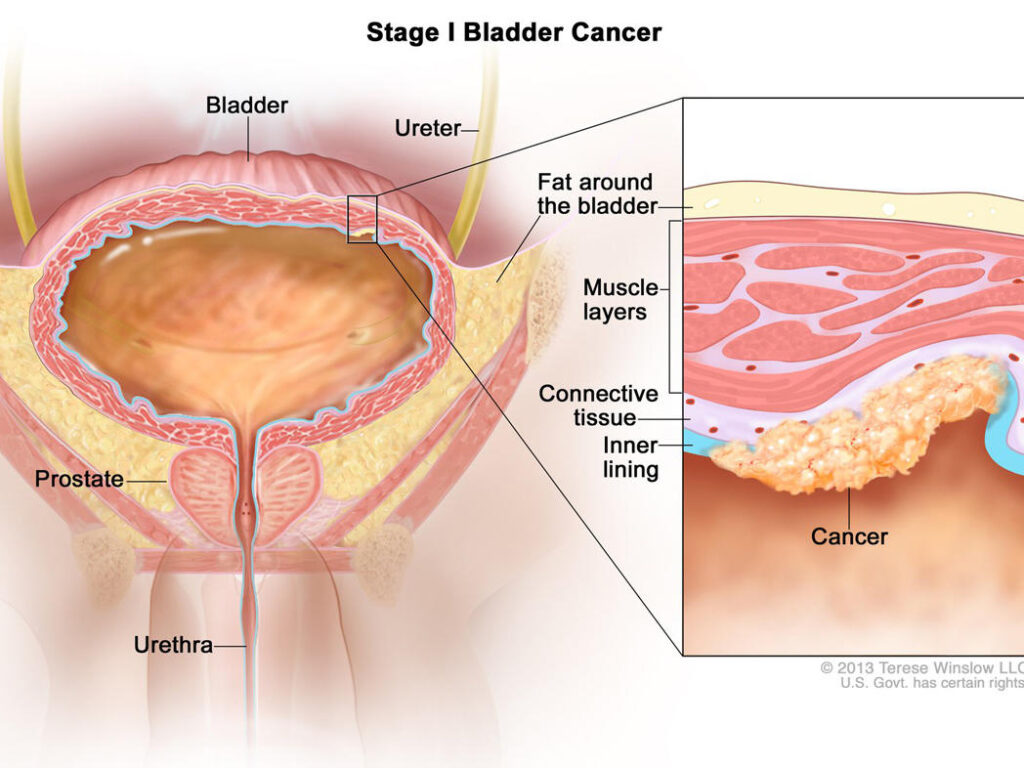
Bladder carcinoma, particularly non-muscle invasive bladder cancer (NMIBC), exhibits one of the highest recurrence rates among all malignancies. Despite complete tumor resection via transurethral resection of bladder tumor (TURBT), recurrence occurs in approximately 50–70% of cases. Preventing recurrent bladder carcinoma requires a multifaceted approach encompassing risk stratification, adjuvant therapies, vigilant monitoring, and modifiable lifestyle factors.
Risk Stratification and Recurrence Predictors
Effective prevention begins with identifying recurrence risk based on tumor characteristics:
| Risk Factor | Impact on Recurrence |
|---|---|
| Tumor size >3 cm | Higher risk |
| Multiple tumors | Increased recurrence probability |
| High-grade histology | Elevated risk of progression |
| Carcinoma in situ (CIS) | Strong recurrence and progression risk |
| Recurrence at first follow-up | Indicates aggressive tumor biology |
| Incomplete initial resection | Facilitates residual tumor regrowth |
EORTC risk tables and CUETO scoring models help guide clinical decisions.
Role of TURBT in Recurrence Prevention
High-Quality Tumor Resection
A meticulous TURBT remains the cornerstone in managing and preventing recurrence. Key surgical considerations include:
- Complete resection of visible tumor and detrusor muscle sampling
- Resection of surrounding mucosa to detect CIS
- Second-look TURBT in high-grade T1 or incomplete resections (within 2–6 weeks)
Intravesical Therapy for Long-Term Prevention
Immediate Postoperative Chemotherapy
Within 24 hours of TURBT, a single instillation of intravesical chemotherapy significantly reduces recurrence risk in low- and intermediate-risk patients.
- Mitomycin C, epirubicin, or gemcitabine are commonly used
- Disrupts micro-residual tumor cells and prevents implantation
Bacillus Calmette-Guérin (BCG) Immunotherapy
For intermediate- and high-risk NMIBC, BCG intravesical instillation is the most effective agent for reducing both recurrence and progression.
- Induction: Weekly for 6 weeks
- Maintenance: Over 1–3 years depending on patient tolerance and recurrence risk
- Efficacy: Up to 70% reduction in recurrence
Chemotherapeutic Maintenance Options
For patients who cannot tolerate BCG or with intermediate-risk NMIBC:
- Maintenance with mitomycin C or epirubicin may reduce recurrence
- Hyperthermic intravesical chemotherapy (HIVEC) is emerging as an adjunct strategy
Surveillance Protocols and Early Detection
Regular follow-up is critical for identifying and managing recurrent disease early:
| Risk Level | Cystoscopy Frequency | Urine Cytology |
|---|---|---|
| Low-risk NMIBC | Every 3 months for 1 year, then yearly | At discretion of urologist |
| Intermediate-risk | Every 3 months for 2 years, then every 6 months | Periodically, especially with CIS suspicion |
| High-risk NMIBC | Every 3 months for 2 years, every 6 months up to 5 years, then annually | Recommended at each visit |
Advanced tools like NMP22, UroVysion FISH, and bladder tumor markers can support standard monitoring.
Lifestyle Modifications to Reduce Bladder Cancer Recurrence
Smoking Cessation
Tobacco use is the most significant modifiable risk factor:
- Carcinogens from smoking are excreted in urine, exposing the urothelium
- Cessation reduces recurrence and improves treatment response
Dietary Interventions
Certain dietary changes may aid in prevention:
- Increased intake of cruciferous vegetables (e.g., broccoli, cauliflower)
- Antioxidant-rich fruits and reduced intake of processed meats
- Adequate hydration to dilute urinary carcinogens
Occupational Exposure Control
Patients with exposure to aromatic amines (e.g., in rubber, dye industries) should be counseled on:
- Proper use of protective equipment
- Potential workplace change
Addressing High-Grade and Muscle-Invasive Risks
Early Cystectomy in Select Patients
High-grade T1 disease unresponsive to BCG may require radical cystectomy to prevent progression.
Upper Tract Surveillance
Patients with recurrent bladder carcinoma also face elevated risk of upper urinary tract urothelial carcinoma. Periodic imaging and urine cytology help early detection.
Future Directions and Immunotherapy Advancements
Emerging therapies aim to improve recurrence prevention while reducing BCG-related toxicity:
- Checkpoint inhibitors (e.g., Atezolizumab, Nivolumab) under evaluation for BCG-unresponsive NMIBC
- Gene therapy (e.g., Nadofaragene firadenovec) delivering IFN-α gene shows promise
- Combination regimens (e.g., BCG + interferon) to enhance immune efficacy
Prevention of recurrent bladder carcinoma hinges on a thorough initial resection, individualized risk stratification, timely administration of intravesical therapy, and consistent long-term follow-up. Combining surgical excellence with medical precision, immunotherapeutic innovation, and lifestyle intervention enables us to significantly reduce the burden of recurrence. By adhering to this integrative model of care, recurrence rates can be minimized, progression risks mitigated, and patient outcomes substantially improved.