Perioperative infections, particularly surgical site infections (SSIs), remain a significant source of morbidity, prolonged hospitalization, and increased healthcare costs globally. Implementing rigorous infection prevention protocols throughout the preoperative, intraoperative, and postoperative periods is essential to enhancing patient safety and surgical outcomes.
Understanding Perioperative Infection
Perioperative infection refers to infections that occur during or shortly after surgical procedures. These include superficial incisional infections, deep incisional infections, and organ/space infections. The most common causative agents are Staphylococcus aureus, Escherichia coli, and Pseudomonas aeruginosa, often introduced through surgical wounds or contaminated instruments.
Risk Factors for Perioperative Infections
- Patient-Related Factors: Diabetes mellitus, obesity, malnutrition, immunosuppression, advanced age, smoking, and pre-existing infections.
- Procedure-Related Factors: Duration of surgery, type of surgery (clean, clean-contaminated, contaminated, dirty), emergency procedures, and use of prosthetic implants.
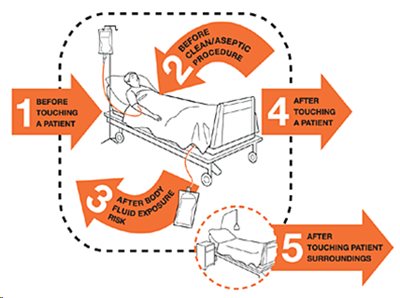
- Environmental and Institutional Factors: Operating room traffic, hand hygiene compliance, sterilization quality, and adherence to aseptic technique.
Preoperative Strategies for Infection Prevention
1. Patient Screening and Risk Assessment
Thorough preoperative evaluation allows clinicians to identify and mitigate individual infection risks. This includes:
- Screening for Staphylococcus aureus colonization and treating with mupirocin and chlorhexidine.
- Optimizing glycemic control in diabetic patients.
- Advising smoking cessation at least 4 weeks before surgery.
2. Preoperative Antiseptic Preparation
- Patients should bathe or shower with chlorhexidine gluconate at least the night before and the morning of surgery.
- Hair removal, if necessary, should be performed using clippers immediately before surgery, never razors.
3. Prophylactic Antibiotic Administration
- Administer appropriate prophylactic antibiotics within 60 minutes before the incision (120 minutes for vancomycin or fluoroquinolones).
- Tailor antibiotic choice to the procedure and likely organisms, ensuring redosing if the operation exceeds two half-lives of the drug.
Intraoperative Measures to Prevent Infection
1. Aseptic Technique and Sterile Field Maintenance
- Strict adherence to sterile technique by all operating room personnel.
- Minimal staff movement and conversation during surgery.
- Use of sterile drapes, gowns, gloves, and properly sterilized instruments.
2. Environmental Control
- Operating room air should be maintained with laminar airflow and HEPA filtration.
- Temperature and humidity must remain within optimal ranges (20–24°C, 50–60%).
3. Surgical Technique Optimization
- Minimize tissue trauma and maintain hemostasis to prevent hematoma formation.
- Avoid devascularization and excessive cauterization.
- Use closed suction drainage only when necessary and remove as soon as possible.
Postoperative Infection Control Measures
1. Wound Care and Dressing
- Maintain a sterile dressing for the first 24 to 48 hours postoperatively.
- Inspect for signs of infection such as erythema, warmth, drainage, or swelling.
2. Glycemic and Temperature Management
- Maintain perioperative blood glucose levels below 180 mg/dL in both diabetic and non-diabetic patients.
- Prevent postoperative hypothermia, as it can impair neutrophil function and wound healing.
3. Surveillance and Early Intervention
- Routine surveillance of surgical sites post-discharge is critical.
- Prompt identification and treatment of infections prevent progression and systemic involvement.
Antimicrobial Stewardship in Surgical Settings
Judicious use of antibiotics is essential to prevent resistance and ensure efficacy. Key principles include:
- Avoid extended postoperative antibiotic use beyond 24 hours for most clean and clean-contaminated procedures.
- Customize prophylaxis based on local microbiological data and resistance patterns.
- Monitor antibiotic effectiveness and adverse effects continuously.
Education, Training, and Audit Practices
Regular training for healthcare workers on infection control guidelines and aseptic practices is fundamental. Furthermore:
- Periodic audits of compliance with infection prevention protocols.
- Use of infection rates as quality indicators to guide performance improvement.
Multidisciplinary Collaboration
Effective infection control demands collaboration between surgeons, anesthesiologists, nurses, infection control teams, and pharmacists. Standardized checklists and bundles improve protocol adherence and outcomes.
A robust and evidence-based perioperative infection prevention protocol not only ensures patient safety but also significantly reduces the burden on healthcare systems. From meticulous preoperative screening and antibiotic timing to intraoperative vigilance and postoperative monitoring, every step plays a pivotal role. Institutions must continue refining and enforcing these practices through training, surveillance, and interdisciplinary collaboration to achieve optimal surgical outcomes.