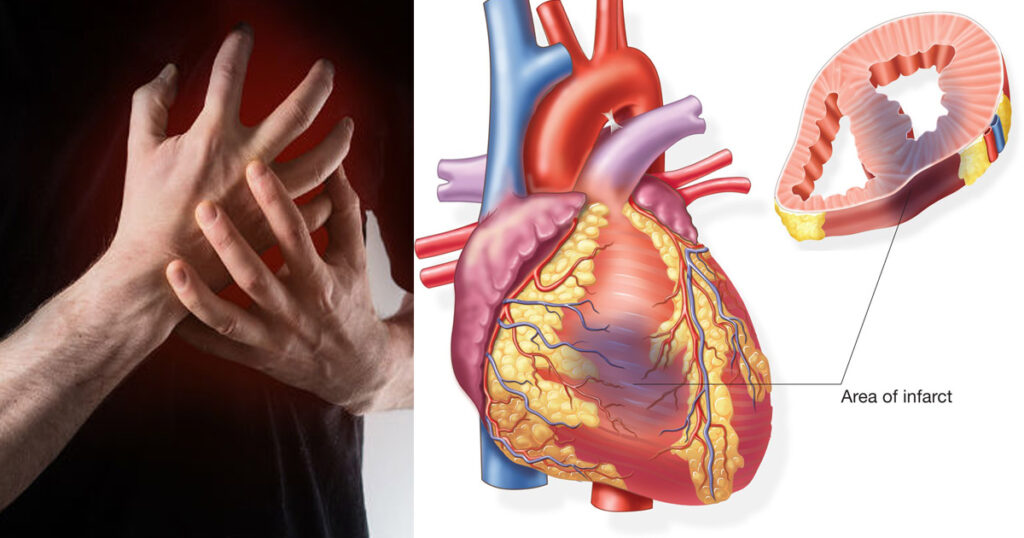
Non-Q wave myocardial infarction (non-Q wave MI), often categorized under non-ST elevation myocardial infarction (NSTEMI), poses significant risk for recurrent ischemic events, including reinfarction, heart failure, and sudden cardiac death. Preventing these complications is critical in optimizing long-term outcomes for affected patients. This article outlines evidence-based strategies for the effective prevention of ischemic complications following a non-Q wave MI.
Understanding Non-Q Wave MI and Its Ischemic Risk
Non-Q wave MI is defined by myocardial necrosis without the development of pathologic Q waves on the electrocardiogram (ECG). Unlike transmural infarctions, these events are often subendocardial and less extensive, yet they carry a considerable risk of ischemic recurrence.
Key Characteristics:
- Typically involves incomplete coronary artery occlusion
- Elevated cardiac troponin levels without significant ST elevation
- Associated with unstable coronary plaques and ongoing ischemia
- Often precedes larger infarctions or sudden cardiac death if untreated
Risk Stratification and Early Intervention Strategy
1. Clinical Risk Scoring Systems
Timely risk stratification enables targeted prevention strategies.
- TIMI Risk Score: Considers age, cardiac markers, ECG changes, and risk factors
- GRACE Score: Provides mortality risk estimation based on age, vitals, creatinine, and ECG
Early identification of high-risk patients allows for prompt invasive evaluation and tailored therapy.
2. Early Invasive Versus Conservative Management
For moderate to high-risk patients, an early invasive strategy is favored.
- Coronary angiography within 24–72 hours for diagnosis and possible percutaneous coronary intervention (PCI)
- Conservative management only in low-risk or comorbidity-constrained cases
Pharmacologic Interventions for Ischemic Complication Prevention
1. Antiplatelet Therapy
Dual antiplatelet therapy (DAPT) remains the cornerstone of secondary prevention.
- Aspirin: Administered immediately and continued indefinitely
- P2Y12 Inhibitors (e.g., clopidogrel, ticagrelor):
- Ticagrelor preferred in ACS for superior efficacy over clopidogrel
- Duration: At least 12 months post-MI, adjusted per bleeding risk
2. Anticoagulation Therapy
Used during acute management to prevent thrombus propagation.
- Unfractionated heparin (UFH) or low molecular weight heparin (LMWH)
- Fondaparinux is an alternative with a lower bleeding profile
- Discontinued post-PCI unless another indication exists
3. Beta-Blockers
Reduce myocardial oxygen demand and prevent arrhythmic complications.
- Initiate within 24 hours if no contraindications (e.g., bradycardia, hypotension)
- Continued long-term in patients with reduced ejection fraction
4. ACE Inhibitors and ARBs
Mitigate left ventricular remodeling and reduce mortality.
- Recommended in patients with LV dysfunction, diabetes, or hypertension
- Start within 24 hours post-MI in stable patients
5. Statin Therapy
Stabilizes plaques and lowers LDL cholesterol aggressively.
- High-intensity statin (e.g., atorvastatin 80 mg daily) initiated early
- Target LDL-C: <70 mg/dL or a ≥50% reduction from baseline
Lifestyle Modification and Risk Factor Optimization
1. Smoking Cessation
- Most significant modifiable risk factor
- Referral to smoking cessation programs and nicotine replacement therapy improves success
2. Diabetes and Hypertension Control
- Target BP: <130/80 mmHg
- Maintain HbA1c: <7% through diet, exercise, and pharmacotherapy
3. Nutritional and Physical Activity Guidelines
- Emphasize Mediterranean-style diet: low in saturated fat, rich in fruits, vegetables, and omega-3s
- Gradual resumption of aerobic exercise after cardiac rehabilitation clearance
Cardiac Rehabilitation and Long-Term Monitoring
Participation in structured cardiac rehabilitation is essential.
- Reduces all-cause mortality and hospital readmission
- Includes exercise training, nutritional counseling, stress management, and medication adherence support
Follow-up should include:
- Regular lipid and glucose monitoring
- Echocardiography to assess left ventricular function
- Ambulatory ECG monitoring if arrhythmia suspected
Surveillance and Management of Recurrent Ischemia
Patients with non-Q wave MI are prone to early recurrent ischemic episodes, necessitating vigilant follow-up.
Warning Signs:
- Recurrent angina, ECG changes, or troponin elevation
- New or worsening heart failure symptoms
Immediate revascularization may be indicated based on non-invasive imaging or repeat angiography.
Frequently Asked Questions:
What is a non-Q wave myocardial infarction?
A non-Q wave MI is a type of heart attack where the ECG does not show Q wave changes, but there is myocardial damage evidenced by elevated troponins.
How is it different from a STEMI?
Non-Q wave MI typically involves partial coronary occlusion and less severe tissue damage than ST-elevation MI, but with a similar risk for complications.
What medications help prevent complications?
A combination of aspirin, P2Y12 inhibitors, beta-blockers, ACE inhibitors, and statins form the backbone of prevention therapy.
Can ischemic complications be completely avoided?
With timely intervention, optimal medical therapy, and risk factor management, many complications can be significantly reduced, though not always fully prevented.
Is cardiac rehab necessary?
Yes. Cardiac rehabilitation significantly reduces the risk of recurrent MI and improves survival and quality of life.
The prevention of ischemic complications following a non-Q wave MI requires an integrated, multi-pronged approach. Combining early risk stratification, appropriate revascularization, evidence-based pharmacologic therapy, lifestyle modification, and long-term surveillance, we can effectively reduce the incidence of recurrent myocardial ischemia, heart failure, and cardiac mortality in this high-risk group. Proactive care coordination and patient adherence to therapy remain vital to long-term success.