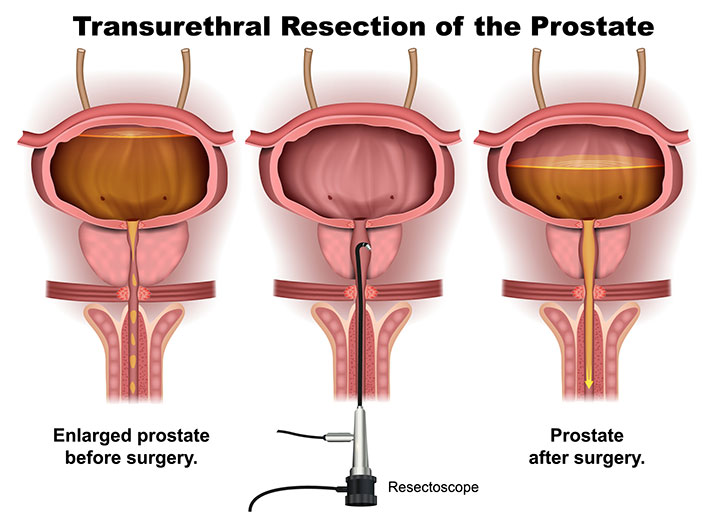
Infections following transurethral surgical procedures remain a notable concern in urological practice. Whether performing transurethral resection of the prostate (TURP), transurethral resection of bladder tumors (TURBT), or other interventions, stringent infection control protocols are imperative. Proper implementation of these measures ensures patient safety, reduces hospital-acquired infections, and minimizes postoperative morbidity.
Understanding Infection Risk in Transurethral Surgery
Transurethral surgery inherently involves instrumentation of the urinary tract, an area colonized by diverse microbial flora. Key routes of infection include:
- Ascending urethral contamination during instrumentation
- Contamination of surgical equipment or irrigating fluids
- Bacterial colonization of indwelling catheters
- Breaks in sterile technique during the procedure
Risk factors amplifying infection susceptibility:
- Pre-existing urinary tract infection (UTI)
- Indwelling catheters
- Diabetes mellitus
- Elderly or immunocompromised status
- Prolonged operative time or incomplete bladder emptying
Preoperative Strategies for Infection Prevention
1. Screening and Treating Asymptomatic Bacteriuria
All patients undergoing transurethral surgery must undergo urinalysis and urine culture prior to the procedure. Detection of bacteriuria necessitates:
- Initiation of targeted antibiotic therapy based on culture sensitivity
- Delay of elective surgery until infection resolution
Failure to treat asymptomatic bacteriuria may result in urosepsis postoperatively.
2. Antibiotic Prophylaxis
Administering prophylactic antibiotics before transurethral procedures significantly reduces postoperative UTI risk.
Recommended Regimen:
- Single dose IV antibiotic 30–60 minutes before surgery
- First-line agents: Cefazolin, Ciprofloxacin, Trimethoprim-Sulfamethoxazole (based on local antibiogram)
- Adjust dose for renal function in elderly patients
Prophylaxis should be short-term to reduce antibiotic resistance development.
Intraoperative Aseptic Measures
1. Strict Aseptic Technique
- Full sterile draping and surgical hand antisepsis
- Use of sterile gloves, gowns, and instruments
- Regular hand hygiene compliance auditing
- Sterile irrigation systems to prevent retrograde contamination
2. Irrigant Sterility and Equipment Maintenance
- Use of sterile water or saline for irrigation
- Avoid prolonged use of open irrigation systems
- Regular disinfection of resectoscopes, cameras, and tubing
Automated washer-disinfectors must be used with validated thermal or chemical disinfection cycles.
3. Bladder Decompression and Controlled Instrumentation
- Maintain continuous bladder drainage to prevent overdistension
- Avoid repeated re-entry and instrumentation
- Limit operative time to reduce mucosal trauma and infection risk
Postoperative Protocols to Minimize Infection Risk
1. Catheter Management
Indwelling catheters are a leading source of catheter-associated urinary tract infections (CAUTIs).
Key Measures:
- Use silicone or hydrogel-coated catheters for reduced biofilm formation
- Maintain a closed sterile drainage system
- Avoid unnecessary catheter use or prolonged placement
- Implement early catheter removal protocols based on patient recovery
2. Bladder Irrigation Protocol
- Perform continuous bladder irrigation (CBI) with sterile fluid only
- Ensure closed system integrity
- Avoid irrigation bottle reuse
- Monitor for signs of infection: cloudy urine, fever, or hematuria with clots
3. Postoperative Surveillance
- Regular monitoring of vital signs and urine output
- Urinalysis or culture if infection is suspected
- Educate patients on hygiene and early signs of infection
Evidence-Based Guidelines and Recommendations
European Association of Urology (EAU)
- Recommends routine preoperative urine culture
- Advocates for short-term prophylaxis over extended antibiotic therapy
- Emphasizes aseptic catheter insertion and maintenance
Centers for Disease Control and Prevention (CDC)
- Urges minimizing catheter duration
- Suggests catheter use only when clinically necessary
- Recommends daily assessment of catheter necessity
Frequently Asked Questions:
What is the most common infection after TURP?
Catheter-associated urinary tract infection (CAUTI) is the most prevalent complication, often due to prolonged catheter use.
Should all patients receive antibiotics before transurethral surgery?
Yes, prophylactic antibiotics significantly reduce the risk of postoperative UTI and are standard care for most transurethral procedures.
Can asymptomatic bacteriuria be ignored?
No. Untreated bacteriuria can escalate to urosepsis post-surgery and must be managed prior to transurethral intervention.
How long should the catheter remain post-surgery?
Catheterization should be as brief as clinically possible, often 1–2 days for uncomplicated TURP or TURBT, with daily reassessment.
What steps can prevent CAUTIs?
Using sterile technique, choosing appropriate catheter types, maintaining closed drainage, and ensuring early removal are key strategies.
Comprehensive prevention of infection from transurethral surgery hinges on a multiphase protocol encompassing preoperative preparation, intraoperative vigilance, and diligent postoperative care. Adhering to evidence-based standards, including urine screening, short-course antibiotic prophylaxis, aseptic catheter handling, and irrigation system sterility, ensures optimal surgical outcomes while minimizing infection risks. A culture of continuous surveillance and patient education further enhances infection control in urological surgery.