Head and neck cancers linked to human papillomavirus (HPV), particularly oropharyngeal cancers, have risen significantly over the past two decades. While tobacco and alcohol have historically been dominant risk factors, HPV—specifically HPV-16—has become the leading cause of oropharyngeal cancer in several regions, including North America and Europe. Preventing these cancers requires a comprehensive strategy, including vaccination, public education, risk reduction, and screening.
Understanding HPV-Related Head and Neck Cancers
Human papillomavirus is a DNA virus that infects epithelial cells and is known to cause several malignancies, including cervical, anal, penile, and oropharyngeal cancers. HPV type 16 accounts for over 90% of HPV-positive head and neck cancers.
Oropharyngeal Cancer and HPV
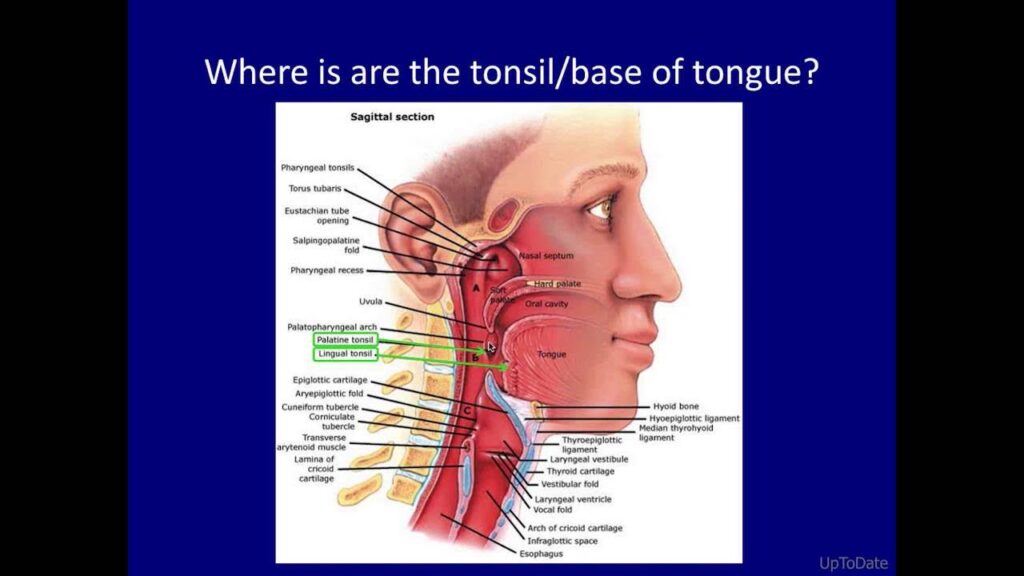
HPV-positive oropharyngeal cancers commonly affect the:
- Tonsils
- Base of tongue
- Soft palate
- Pharyngeal walls
These cancers are biologically distinct from HPV-negative tumors, often occurring in younger individuals with no history of smoking or heavy alcohol use. HPV-associated cancers typically respond better to treatment and have improved prognoses.
HPV Vaccination: A Critical Preventive Measure
Available HPV Vaccines
The cornerstone of prevention is prophylactic HPV vaccination, which targets high-risk strains of the virus. Approved vaccines include:
- Gardasil-9 (nonavalent): Protects against 9 HPV types, including 16 and 18
- Cervarix (bivalent): Protects against HPV 16 and 18
Both vaccines are effective in preventing infection with the HPV types most associated with head and neck cancer.
Recommended Vaccination Schedules
- Ages 9–14: Two doses, 6–12 months apart
- Ages 15–26: Three doses over 6 months
- Ages 27–45: Vaccination based on shared clinical decision-making
Early vaccination—ideally before the onset of sexual activity—is critical to achieving optimal protection.
Impact of HPV Vaccination on Head and Neck Cancer Incidence
Evidence shows that widespread HPV vaccination reduces oral HPV prevalence, which correlates with future reductions in HPV-related cancers.
Key Findings:
- Oral HPV16/18 prevalence declined by over 80% among vaccinated individuals
- Herd immunity has led to a decline in oral HPV even in some unvaccinated males
- Modeling predicts significant decreases in oropharyngeal cancer cases over the next few decades with sustained vaccine coverage
Raising Public Awareness and Education
Addressing Vaccine Hesitancy
Misinformation and social stigma contribute to suboptimal vaccine uptake. Public health campaigns must:
- Emphasize the cancer-preventing potential of the HPV vaccine
- Clarify that both males and females benefit
- Promote inclusion of the vaccine in routine adolescent immunization
School-Based and Community Outreach
Integration of HPV vaccination into school health programs is proven to increase access and uptake, especially in underserved populations. Outreach in universities, sports teams, and healthcare clinics also plays a crucial role.
Behavioral Risk Reduction Strategies
Safe Sexual Practices
Since HPV is primarily transmitted through sexual contact, public health education should promote:
- Use of barrier protection methods (e.g., condoms, dental dams)
- Limiting the number of sexual partners
- Open communication about HPV risks and vaccination
Tobacco and Alcohol Cessation
While HPV is a major cause, tobacco and alcohol remain synergistic risk factors for head and neck cancers. Reduction or cessation:
- Decreases the likelihood of co-factor induced carcinogenesis
- Improves outcomes for those undergoing treatment for HPV-related cancers
Screening and Early Detection in High-Risk Groups
Currently, there is no standardized screening test for HPV-related oropharyngeal cancer. However, clinicians should maintain heightened vigilance in individuals with:
- Persistent sore throat, hoarseness, or difficulty swallowing
- Enlarged cervical lymph nodes
- History of multiple sexual partners
- Known exposure to HPV or lack of vaccination
Biomarker-based methods, including salivary HPV DNA detection, are under investigation for future screening protocols.
Gender-Inclusive Prevention Strategies
Originally targeted toward females, HPV vaccination now includes routine immunization for males, who are disproportionately affected by oropharyngeal cancers. Equal access to vaccination ensures:
- Direct protection for males
- Reduced transmission to sexual partners
- Strengthened population-wide immunity
International and National Policy Implementation
Global initiatives such as the WHO’s Global Strategy to Accelerate the Elimination of Cervical Cancer also encompass head and neck cancer prevention via:
- Vaccine introduction in low- and middle-income countries
- Support for national immunization programs
- Alignment with UN Sustainable Development Goals
Frequently Asked Questions
Can the HPV vaccine prevent head and neck cancer?
Yes. The HPV vaccine prevents infection with the high-risk types of HPV that cause oropharyngeal and other head and neck cancers.
Should boys get the HPV vaccine?
Absolutely. Males are at significant risk of developing HPV-related oropharyngeal cancers. Vaccinating boys contributes to individual and herd protection.
Is there a screening test for oral HPV?
Currently, no routine screening test exists for oral HPV infection. Research is ongoing to develop saliva-based diagnostics for early detection.
What age is best for HPV vaccination?
Vaccination is most effective when administered before exposure to HPV, ideally between ages 9 and 14.
Does smoking increase the risk of HPV-related head and neck cancer?
Yes. Smoking can synergize with HPV to increase cancer risk and worsen treatment outcomes.
Preventing head and neck cancer due to human papillomavirus requires a robust, multifaceted approach. Vaccination remains the most effective strategy, supported by community education, behavioral change, and policy initiatives. As vaccination coverage expands and research advances, the global burden of HPV-related oropharyngeal cancers will continue to decline. Let us invest collectively in immunization and awareness to protect current and future generations from this preventable disease.

